Background: Patients are often discharged from the hospital with active medical issues needing outpatient follow-up (AINF) – including recommended labs, imaging, procedures, follow-up appointments, and follow-up of incidental findings – but patients and their outpatient providers often fail to complete these recommended workups [1]. Primary care physicians strongly recommend that discharging providers include a brief list of AINF in one dedicated area at the top of the provider-facing discharge summary [2] , but in the patient-facing written discharge plan (after hospital care plan or AHCP) AINF are often not included or not organized in a patient-centered way.
Purpose: Our aim was to improve the communication of AINF to patients being discharged from general medicine teaching services (GMED) by encouraging discharging providers to incorporate a patient-centered list of AINF in the AHCP.
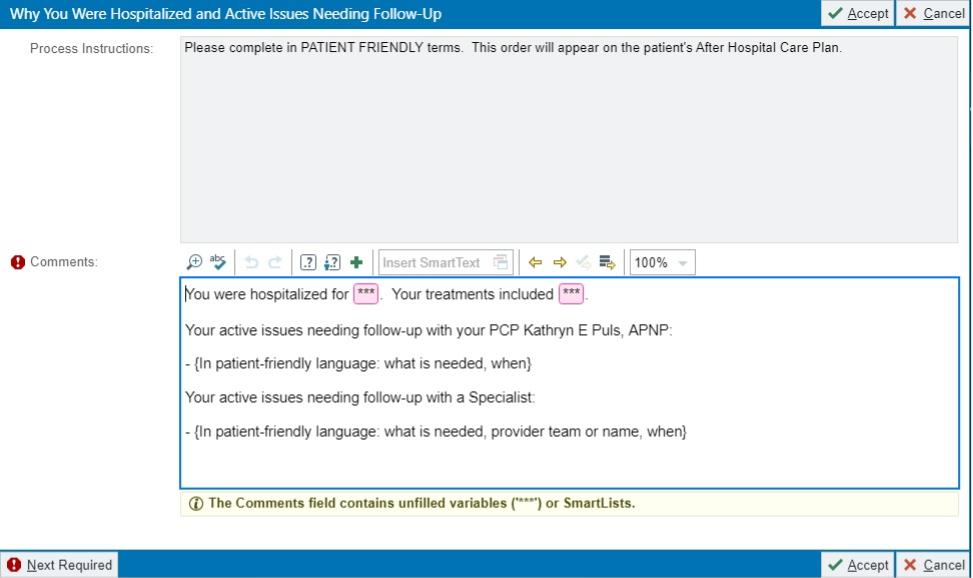
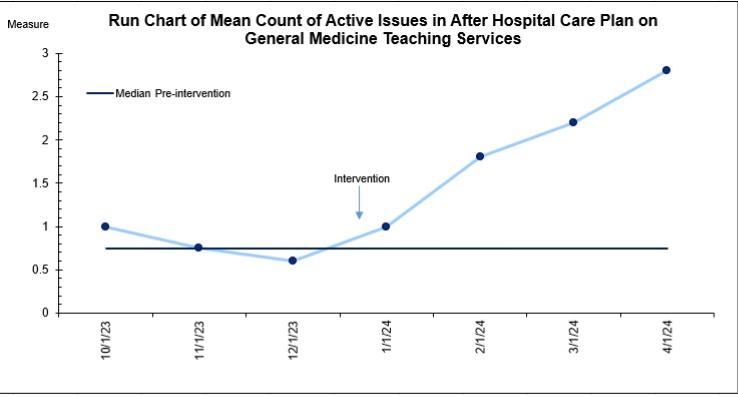
Description: A prompt (figure 1) was added to the discharge orders populating the AHCP that encouraged discharging providers to document a patient-centered list of AINF. Two PDCA cycles testing different versions of this prompt were piloted on non-teaching hospitalist services before implementation on GMED in January 2024. We measured the number of active issues needing follow-up documented anywhere in the AHCP and discharge summary in a random sample of 35 patients discharged from GMED pre-intervention and post-intervention (from October 2023 – April 2024). Pre-intervention, only 27% of the AINF documented in discharge summaries were included in AHCPs; this improved to 67% post-intervention. The mean number of AINF included in the AHCP increased from 0.79 pre-intervention to 1.95 post-intervention. A run chart of the mean number of AINF in the AHCP by month shows an upward trend post-intervention (figure 2).Residents working on GMED were surveyed post-intervention (n=44) and the majority believed that the enhancement of the AHCP improved patient understanding of their medical issues and follow up needs (79.5%) and would improve adherence to follow up (65.9%). A majority felt that this additional prompt did not disrupt normal workflow (77.3%).
Conclusions: A simple prompt in the discharge orders led to improved documentation of AINF in the patient-facing AHCP, empowering patients to take ownership of their follow-up care in a patient-centered way. Next steps include assessing how the quality of AINF documentation in the AHCP impacts patient understanding of their AINF, adherence to recommended follow-up, and readmission rates.