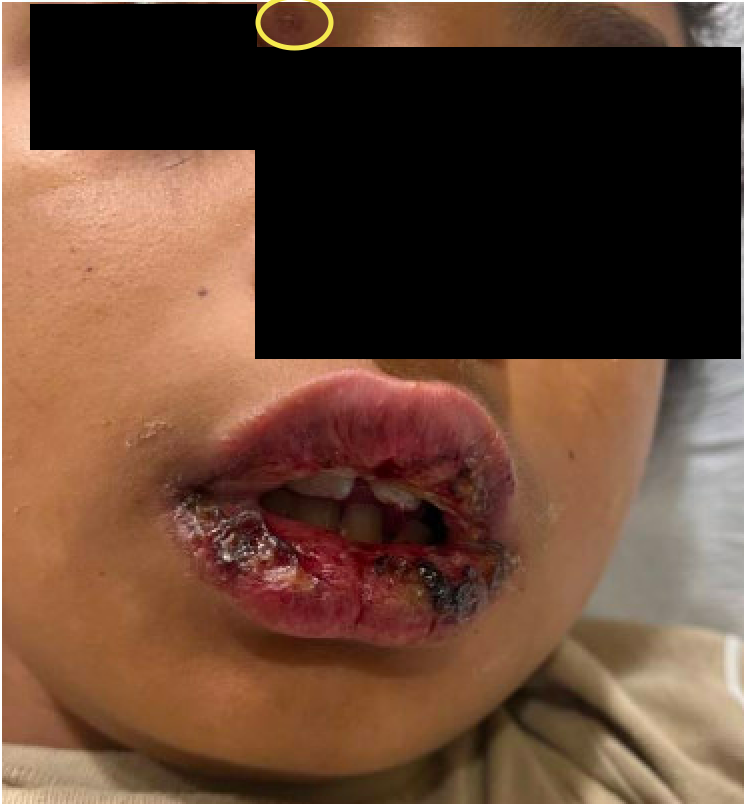
Case Presentation: An 8-year-old boy presented with 8 days of lip swelling, crusting, peeling, and bleeding, causing poor oral intake and dehydration. Initial symptoms included cough, nasal congestion, and fever (100.4°F). He developed lip ulcerations and was seen multiple times with diagnosis of oral herpes and impetigo superinfection. After 4 days of adequate herpes/impetigo therapy, his symptoms progressed, with new skin lesions on his ears and near his right eye, and worsening, hemorrhagic lip findings. Exam was notable for persistent wet cough, trismus, erosions of the lips and urethral meatus, vesiculobullous lesions near his right eye and on/behind his ears, and hypopigmented limb lesions. There were no visible tongue lesions. Chest X-ray was unremarkable. Infectious testing was positive for rhino/enterovirus, negative for HSV. He was diagnosed with RIME (reactive infectious mucocutaneous eruption) and improved with methylprednisolone and azithromycin treatment. At an 8-day dermatology follow-up, only minor lip erosions remained.
Discussion: RIME, first described in 2015, is a rare inflammatory condition marked by mucosal erosions and cutaneous eruptions, typically following a bacterial or viral infection. It is most associated with Mycoplasma pneumoniae, although identifying the specific infectious trigger can be challenging, as seen in this case where Mycoplasma testing was negative despite suspicion of infection. Patients often present with 1 week of prodromal infectious symptoms prior to mucocutaneous findings. Typically, 2-3 mucosal areas are affected, with oral lesions typically including hemorrhagic crusting of the lips. Cutaneous lesions are more varied, though usually vesiculobullous, and have a sparse distribution on the extremities, face, and/or trunk. Systemic corticosteroids are the cornerstone of treatment to control inflammation, and antibiotics may be added when bacterial superinfection is suspected. In this case, azithromycin was used despite his negative mycoplasma test, given his cough, diagnosis of RIME, and known high mycoplasma transmission in the community. Distinguishing RIME, Stephens-Johnson Syndrome (SJS), and herpes gingivostomatitis requires carefully evaluating the clinical history and physical findings. As compared to SJS, RIME is characterized by milder cutaneous involvement and lacks extensive epidermal detachment or association with medication use. Herpes gingivostomatitis involves similarly painful oral lesions, but typically lacks widespread mucosal erosions or skin eruptions seen in RIME and SJS. Recognizing these patterns can guide appropriate treatment.
Conclusions: Hospitalists should have a narrow differential for hemorrhagic lip crusting, including RIME, and be able to elicit an appropriate trigger history to guide appropriate diagnosis and treatment. RIME is triggered by viral or bacterial infections, particularly Mycoplasma, and associated with mucosal and mild cutaneous findings. Early recognition and corticosteroid therapy are critical to managing inflammation and preventing complications.