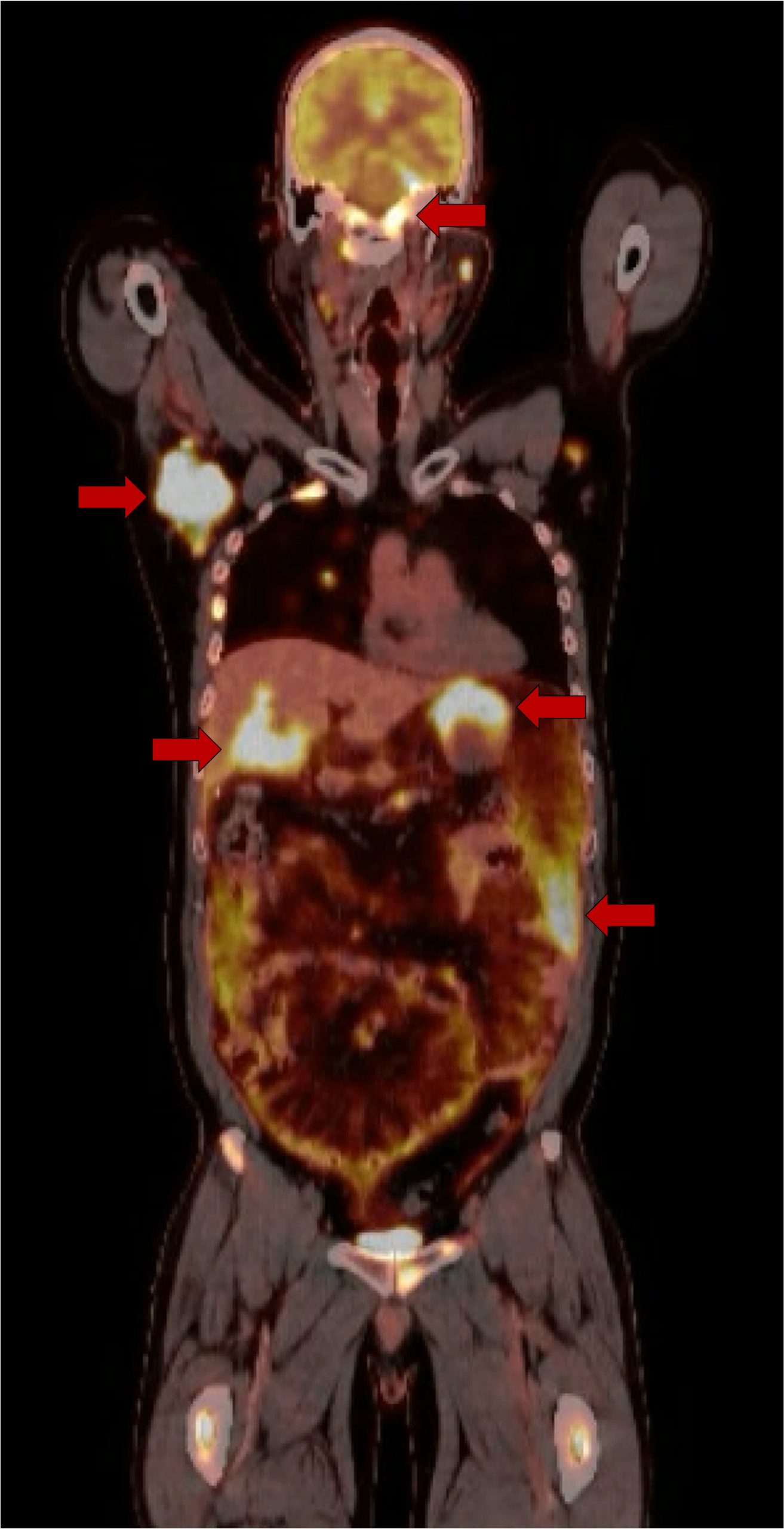
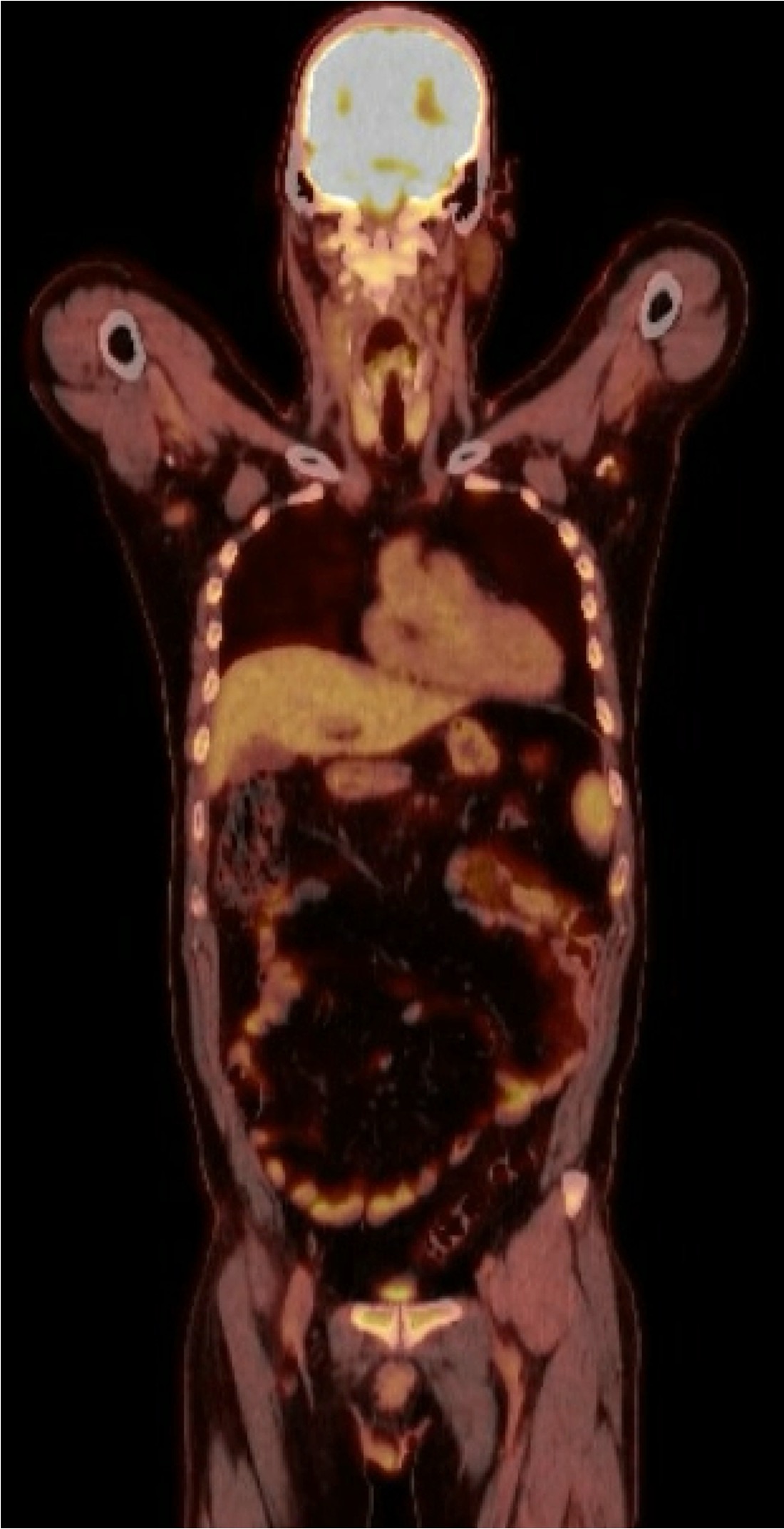
Case Presentation: A 50-year-old male with history of HIV with undetectable viral load on ART presented to the emergency department for evaluation of left eye blurriness, ptosis, and ophthalmoplegia. History was notable for emergency department and outpatient ophthalmology visits one month prior resulting in a diagnosis of cranial nerve six palsy. MR angiography was unremarkable. He developed difficulty opening his left eye and reported having weight loss over the past month. On exam, vital signs were within normal limits. Labs revealed uric acid 8.0 mg/dL and WBC 9.34 K/uL. Repeat orbital imaging showed infiltrative soft tissue throughout the cavernous sinuses. MRI of the brain and positron emission tomography revealed widely distributed lesions and lymphadenopathy throughout the brain, chest, abdomen, pelvis, and skeleton suspicious for malignancy. Bone marrow and lymph node biopsy revealed B cell lymphoma, CD10+/CD5- lambda monotypic. Cytogenetic analysis revealed IGH::MYC rearrangement. Pathology confirmed diagnosis of Epstein-Barr virus (EBV) negative Burkitt lymphoma (BL). Patient began chemotherapy with Etoposide phosphate, Prednisone, Vincristine sulfate (Oncovin), Cyclophosphamide, Doxorubicin hydrochloride (Hydroxydaunorubicin), and Rituximab (EPOCH-R). Follow up 6 months later shows continued response to therapies.
Discussion: HIV is a known carcinogen for many different types of cancer, including so-called “AIDS-defining cancers” (ADCs) like Kaposi sarcoma and non-ADCs (NADCs) like cervical cancer [1]. In the modern ART era, the risk of cancer is still elevated in people living with HIV (PLWH) compared to the general population. In 2017, a study of 448,258 HIV-infected individuals showed PLWH have a standardized incidence ratio (SIR) of 1.69 for cancer compared to the general population (ADC 14.0, NADC 1.21) [2]. Introduction of ART has decreased the burden caused by ADC but has increased the burden caused by NADC [3,4]. Specifically, Burkitt lymphoma and Hodgkin lymphoma have been noted in the literature to occur paradoxically in patients with higher CD4 counts (e.g. >250 cell/mcL) [3,5]. Our patient presented with an undetectable viral load, CD4 count of 776 four days prior, and an incomplete earlier infectious workup. His history of cancer and HIV should have prompted a higher clinical suspicion for cancer given the chronic, ominous progression of symptoms. His ultimate diagnosis of EBV-negative BL highlights the importance of investigating cancer etiologies in the absence of positive serology.
Conclusions: Patients with HIV are at increased risk of malignancy due to alterations in their immune system. Evaluation of atypical illness should include early imaging and biopsy. Preventive actions include thorough routine history and physical (including skin and mucosal exams), optimization of HIV treatment, and comprehensive vaccination (HBV, HPV, VZV).