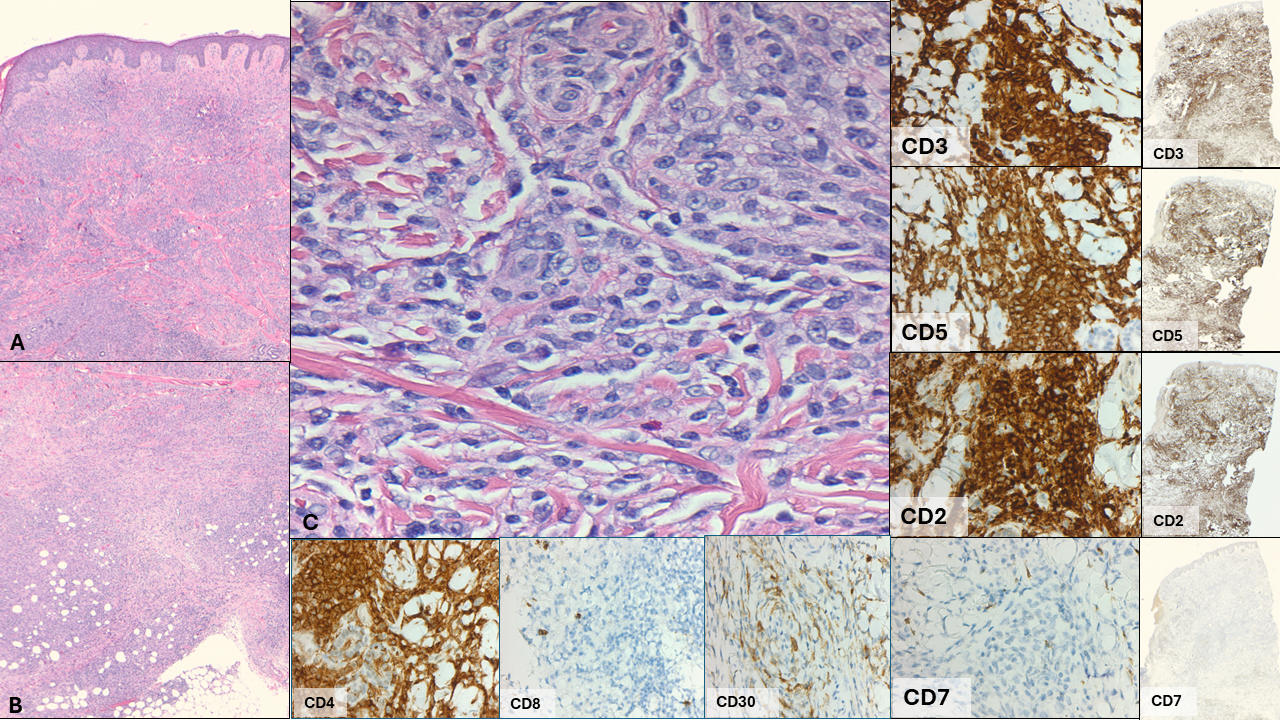
Case Presentation: A 42 year old female with a 5-year history of biopsy-proven eczema presented with two weeks of worsening body pain and skin ulcerations (Figure 1). Six months prior to presentation, she was started on topical steroids and Dupixent without significant improvement. Two months prior to presentation, worsening eosinophilia was noted. On arrival, she was febrile to 101.8 F and tachycardic. Laboratory studies showed white blood cell (WBC) 11.4 K/uL, absolute eosinophil count 1.74 K/uL, lactate 2.5mmol/L, and human T-Cell lymphotropic virus (HTLV) 1 and 2 negative; blood cultures and a wound swab grew methicillin-sensitive staphylococcus aureus (MSSA). Broad spectrum antibiotics were initiated. Chest x-ray was unremarkable. Transthoracic echocardiogram (TTE) was negative for vegetation. Due to persistent fevers and eosinophilia, there was concern for underlying malignancy. Blood flow cytometry showed 50% CD4+ T cells with complete loss of CD7 suggesting a T-cell neoplasm. Sezary smear showed no Sezary cells, and peripheral smear was negative for dysplastic cells. Skin and inguinal lymph node biopsies confirmed mycosis fungoides (Figures 2). Bone marrow biopsy showed no evidence of T cell lymphoma. Positron emission tomography (PET) demonstrated extensive superficial soft tissue hypermetabolic lesions and multiple hypermetabolic lymph nodes representing diffuse lymphomatous involvement. Treatment with gemcitabine was started and, in combination with routine wound care, resulted in gradual clinical improvement.
Discussion: Mycosis fungoides (ΜF) is one of the most common subtypes of cutaneous T cell lуmphomа (СTCL). MF is a mature T cell non-Hodgkin lymphοmа with a heterogenous cutaneous presentation, including patches, plaques, generalized erythroderma, alopecia, and tumors that can involve any body surface; extracutaneous disease can include the lymph nodes, blood, and viscera. While eczema does not progress to MF, the clinical and histological characteristics are often very similar, particularly with early MF, and frequently result in misdiagnosis; this is often compounded by the low incidence of MF (6 cases per million) and its indolent progression. Eosinophilia can occur in both severe eczema and CTCL, as both conditions involve significant skin inflammation. In eczema, eosinophils are often present in lesions, with higher counts correlating with greater disease severity. In CTCL, eosinophilia is less common but may be seen in advanced stages and is associated with more aggressive disease. Patients with eczema typically have a relapsing-remitting course, and the presence of B symptoms and/or refractory lesions should prompt investigation for a malignant process.
Conclusions: MF is a subtype of CTCL and shares clinical and histological features with common benign skin conditions, such as eczema and psoriasis, often resulting in delayed diagnosis. High suspicion for CTCL should be maintained in patients with treatment-refractory eczema and/or associated B symptoms. Lastly, a multidisciplinary approach is often essential in establishing the diagnosis and coordinating treatment.