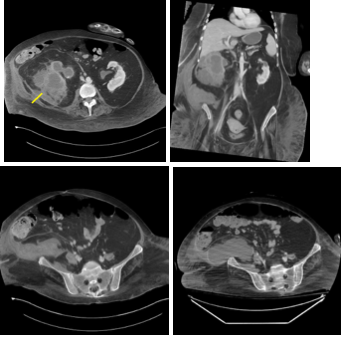
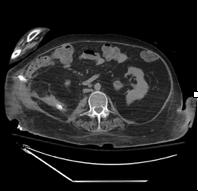
Case Presentation: A 56-year-old female with history of spastic quadriplegia secondary to multiple sclerosis, neurogenic bladder with a long-term indwelling suprapubic catheter presented with septic shock. Labs revealed leukocytosis and lactic acidosis. A contrast enhanced computed tomography of abdomen and pelvis revealed a multiloculated large right renal abscess with staghorn calculus extending into the right retroperitoneum consistent with a diagnosis of xanthogranulomatous pyelonephritis. The renal abscess was initially treated with ceftriaxone, metronidazole and percutaneous drainage. Her cultures from the abscess grew Proteus mirabilis. Patient did not show any improvement in the follow up imaging and required laparotomies with staged debridements. Three surgeries were needed culminating in a right sided nephrectomy. Her operative cultures grew Proteus mirabilis, Pseudomonas and Achromobacter. The patient was treated with meropenem and followed till improvement of her abscess.
Discussion: Xanthogranulomatous pyelonephritis (XGP) is a rare and severe form of kidney inflammation characterized by the accumulation of lipid laden macrophages (xanthoma cells) and granulomatous tissue in the kidney. It typically results from chronic urinary tract obstruction, often due to staghorn calculi. Urine cultures usually yield Escherichia coli and Proteus mirabilis. However, Pseudomonas and Klebsiella have also been cultured.Complications can frequently occur in the form of psoas abscess, nephrocutaneous fistulas, nephrocolonic fistulas and paranephric abscesses. Computed tomography remains the mainstay for diagnosing XGP. However, the definitive diagnosis can only be suggested pathologically with findings of the characteristic xanthoma cells. Treatment includes antibiotic therapy and total nephrectomy – although nephron sparing surgery such as partial nephrectomy can sometimes be attempted. Our patient’s primary risk factors included quadriplegia with neurogenic bladder necessitating the use a chronic suprapubic catheter. Xanthogranulomatous pyelonephritis was diagnosed through a CT abdomen and had already evolved to a retroperitoneal abscess. Antibiotic treatment and multiple drains were placed with hopes to decrease the size of the abscess, but this did not resolve her complicated infection and led to further colonization with multi drug resistant organisms. Ultimately the patient had to undergo right sided nephrectomy.
Conclusions: Xanthogranulomatous pyelonephritis is a rare form of chronic pyelonephritis which is often associated with chronic infection and nephrolithiasis.It occurs due to obstructive uropathy that leads to a cycle of infection and inflammation which ultimately leads to fibrosis and xanthoma cells replacing the renal parenchyma. Early diagnosis is imperative in treating XGP, as it can often complicate situations by involving adjacent structures or organs. Most times, it is diagnosed often after loss of renal function in the affected kidney. Early intervention with a nephrectomy is the treatment of choice to prevent further complications such as perinephric and retroperitoneal abscesses, fistula formation and death.