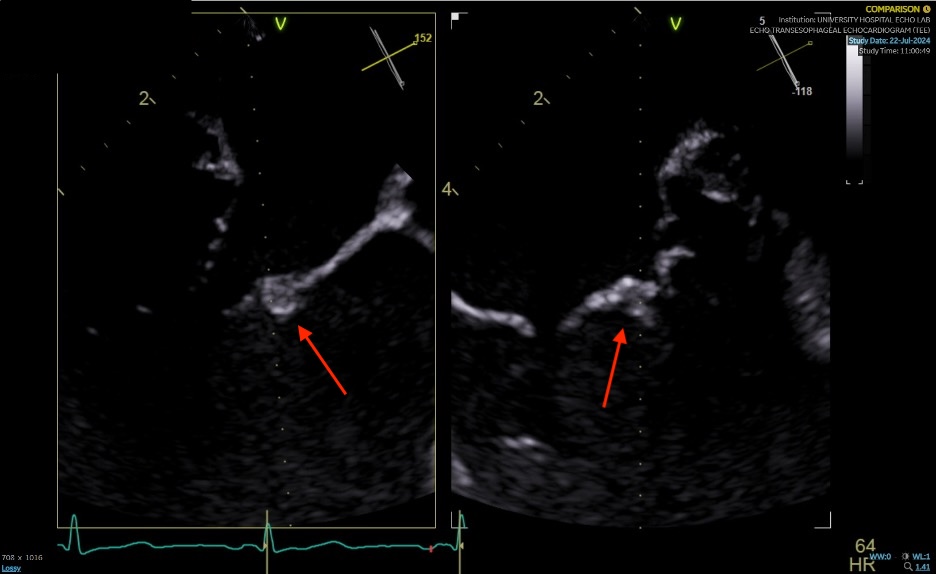
Case Presentation: A 56-year-old male with history of opioid and cocaine use disorder without intravenous drug use presented to the emergency room with bilateral lower extremity swelling and shortness of breath for two weeks. A transthoracic echocardiogram was performed which showed an ejection fraction of 45%, grade II diastolic dysfunction, and severe aortic regurgitation. The patient was diagnosed with new-onset heart failure with reduced ejection fraction. Follow-up transesophageal echocardiogram for aortic insufficiency showed small mobile echodensities on the aortic and mitral valves which likely represent vegetations versus torn chordae, severe aortic regurgitation, and mild mitral regurgitation. The patient developed one episode of fever up to 101 degrees Fahrenheit while hospitalized. Infectious disease was consulted, and prior to starting empiric antibiotics, six blood cultures were collected which all resulted as negative. All other comprehensive infectious workup was negative. After diuresis, the patient was discharged to a rehabilitation facility with a several week course of antibiotics. Two months later, he presented to the emergency department with worsening shortness of breath. Cardiothoracic surgery was consulted and the patient underwent aortic valve replacement. The excised valve was sent out for pathology which showed myxoid change and was negative for organism growth. Given the negative thorough infectious workup and pathology findings, the patient was diagnosed with myxoid degeneration of the aortic valve causing severe aortic insufficiency. Throughout his treatment course, he was started on guideline-directed medical therapy and returned to his rehabilitation facility with an improvement in symptoms.
Discussion: Myxoid degeneration of heart valves most commonly occurs in the mitral valve. Involvement of the aortic valve is typically seen in older patients with an average age of around 63 years old and is thought to be secondary to long-standing systemic hypertension. Diagnosis of cardiac masses such as myxoma are differentiated based on location of the mass, clinical presentation, and appearance on imaging such as on transthoracic or transesophageal echocardiogram, cardiac CT, cardiac MRI, or biopsy. In this case, the patient’s history of polysubstance use, presence of fever, and multiple valvular masses initially pointed toward a diagnosis of bacterial endocarditis. His presentation met one major and one minor criteria of the modified Duke criteria which indicate possible infective endocarditis. However, the lack of reported intravenous drug use, leukocytosis, elevated inflammatory markers, other signs of sepsis, positive blood cultures or other infectious workup, and pathology findings suggested an alternative diagnosis of myxoid degeneration. The development of heart failure was attributed to severe aortic insufficiency from the degenerative change.
Conclusions: The differentiation of valvular abnormalities can be difficult to differentiate even on transthoracic echocardiogram. To diagnose infective endocarditis, one must consider both imaging and pathologic findings along with infectious workup. For those whom the diagnosis is unclear, a high degree of clinical suspicion may warrant treatment with empiric antibiotics while being evaluated for surgical evaluation and pathology.