Background:
Previous studies examining continuous patient monitoring in the ICU and emergency department suggest that substantial telemetry alarm burden combined with a high proportion of false positive alerts may jeopardize patient outcomes. Currently, little is known about the burden and value of specific alarms on the general wards.
Methods:
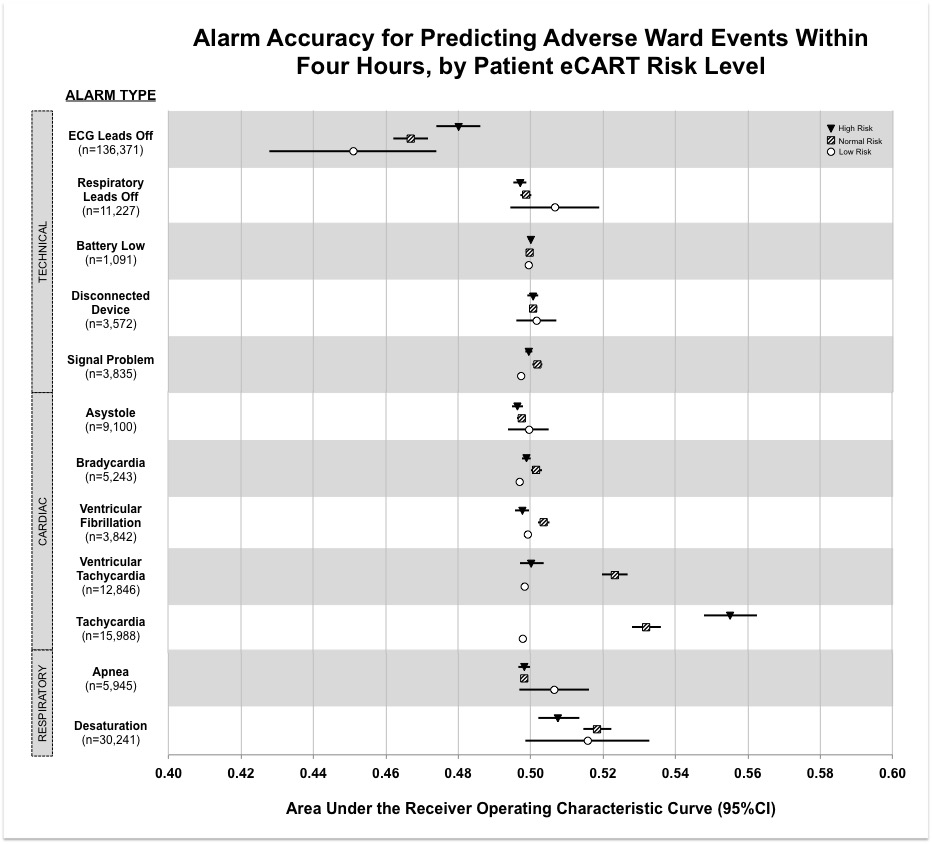
As part of a quality improvement initiative, we conducted a retrospective analysis of unique telemetry alarms generated during consecutive adult medical and surgical general-ward admissions from November 2014 through March 2015 at a 550-bed urban US teaching hospital. We compared the accuracies of individual alarm types for predicting adverse events (specifically RRT activation, intensive care unit transfer, ward cardiac arrest, or in-hospital death) within four hours of a telemetry alarm using area under the receiver operating characteristic curves (AUCs). We performed a sensitivity analysis comparing alarm accuracy between dynamically adjusting Low, Normal and High Risk patient strata, using a previously published risk score, eCART, with thresholds set a priori at <35, 35-50, and >50 respectively.
Results:
Over the study period, a total of 8,292 (69%) patients generated 239,301 ward telemetry alarms at a rate of 6.3 alarms per patient bed-day. Patients who generated ward telemetry alarms were older (59 vs. 51 years, p<0.001), had a longer median ward length of stay (3 vs. 2 days, p<0.001), and were more likely to die before hospital discharge (1.6% vs. 0.4%, p<0.001) than patients who did not generate alarms. The majority of the alarms were technical in nature [n=156,096 (65%)], followed by cardiac [n=47,019 (20%)], and respiratory [n=36,186 (15%)]. Most alarms had poor accuracy for predicting adverse events (Figure). Tachycardia alarms were the most accurate positive predictor [AUC 0.54 (95%CI 0.54-0.55)] overall and ECG leads off alarms were the most accurate negative predictor [AUC 0.46 (95%CI 0.45-0.46)]. Analysis across risk strata demonstrated that the predictive ability of tachycardia alarms was limited to normal and high-risk patients.
Conclusions:
Telemetry monitoring results in a considerable alarm burden on the general wards, with most alarms failing to predict clinically meaningful outcomes. Tachycardia alarms have the strongest correlation with clinical deterioration, whereas ECG leads off alarms signal a decreased risk. Our finding that tachycardia alarms were most accurate in higher risk patients suggests that adjusting alert thresholds by patient severity of illness may improve the validity of alarms. Adjusting alarm parameters in this targeted fashion using real-time patient risk stratification may reduce alarm burden and avoid a one-size fits all approach to alarm management.