Background: Morbidity and Mortality Conference (MMC) has been recognized as a valuable educational resource in training programs to improve patient safety. Traditional MMCs are often poorly defined in terms of format, goals, and outcomes, leading to ineffective reflection, discussion and action. Increasing evidence suggests that a structured and transparent approach to MMCs results in measurable gains in staff satisfaction and participation, education and quality of patient care. In August 2018, our residency program appointed an MMC Faculty Champion (FC) to redesign our monthly MMCs presented by PGY-3 residents. MMC FC reviewed the literature and met with healthcare leaders to develop a new guideline.
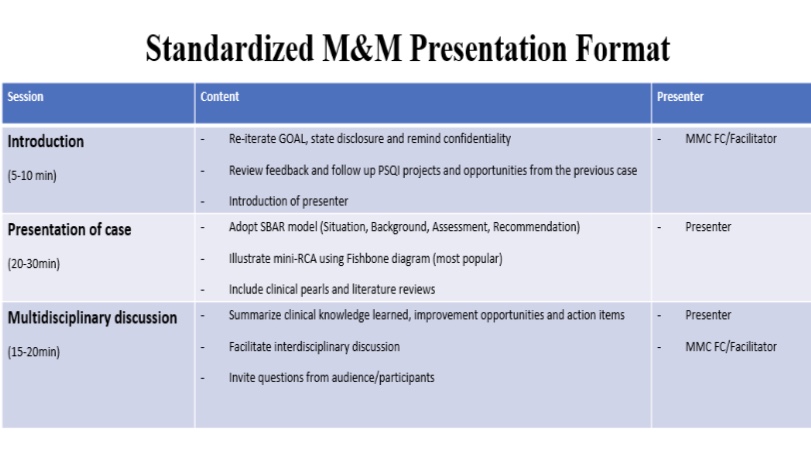
Purpose: Under the new guideline, case selection and preparation processes start 4-6 weeks prior to the presentation. Collaboration with Risk Management (RM) and Quality & Patient Safety (QPS) departments plays a key role in eliminating bias and information gaps during the process of RCA. Progress reports on Patient Safety and Quality Improvement (PSQI) projects generated from prior MMC are presented at the beginning of each conference. A standardized case presentation format features a combination of A3 problem-solving methodology and fishbone diagrams based on the Joint Commission RCA types, focusing on topic learning and system improvement opportunity. A collaborative and non-judgmental approach was adopted for a 20-minute, multidisciplinary discussion following the case presentation. Core attendees include Medical Specialists, Intensivist, Supportive teams, Nursing team, ED Care Coordinators, RM, QPS, Clinical Informatics and Pharmacy. The numerous projects generated have prompted us to establish an MMC Process Improvement Team to more effectively generate and conduct PSQI projects in addressing preventable patient safety events at the hospital and system level. We have identified more than 25 proposed system improvement interventions within 9 months. Our MMC is ACCME accredited.
Description: To assess the effectiveness of our MMC changes, we conducted a survey with 47 faculty and resident responses. Forty two out of 47 (89.13%) reported that the new M&M format has significantly improved this teaching conference, 47/47 (100%) agreed that the multidisciplinary discussion sessions were valuable, 43/47 (91.39%) reported better understanding in system improvement processes as a result of MMC, 42/47 (89.36%) expressed better understanding of RCA process, 45/47 (95.74%) pointed out that the follow up recaps and take home messages were useful, Even more importantly, 42/47 (89.36%) reported seeing positive changes in patient care processes. Changes include better participation and communication, increased awareness of easily missed events and improved EMR functionality. Additional comments include appreciation of the more organized nature of MMC, residents are better-prepared, excellent team effort and a culture shifted away from individual blame/shame.
Conclusions: In summary, we present a program innovation that dramatically transformed our routine MMC into a conference of educational value and system improvement. The significant progress we made demonstrated the importance of collective effort in the structure-process-system-outcome chain. Our conferences provide platforms and opportunities for participants to improve quality of patient care in a safe and nurturing environment. Programs looking to improve their own MMCs might benefit from our experience.