Background: Event reporting has been the cornerstone of patient safety culture since the IOM report “To Err is Human” was published. Over the past 20 years, the medical literature has focused on improving the overall rates, but not the quality, of reporting. To inform change, event reports must have a standard quality of content for use in hospital patient safety efforts.
Purpose: The purpose of this study is to test the impact of a practical and measurable intervention to improve the structure and content of event reports submitted by physician trainees.
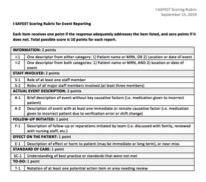
Description: The study involved a one-hour didactic session for Internal Medicine residents delivered during protected educational time. The teaching module was developed with a multidisciplinary team of patient safety leaders. The session included the following:1. Pre-course survey and event report (10 minutes): We collected data on respondents’ reporting habits and experience. Additionally, residents read a fictitious patient safety event of a narcotic overdose and were asked to write an event report.2. Interactive case-based course (40 minutes): We included education on the value of event reporting, what happens to reports, and what constitutes a good or bad report. We also walked through a framework for event reporting using a safety event that involved a delay of antibiotic administration.3. Post-course survey and event report (10 minutes): Residents applied their knowledge by writing a post-course event report for a case involving patient misidentification.The primary measure of the study was the quality of event reporting practices using a comparison of pre- and post-course event reports. Reports were scored using a novel 10-point rubric based on the I-SAFEST model, which was adapted by our team using additional patient safety guidelines. The rubric included items such as event description, staff involved, and action items. The event reports were graded by two independent reviewers and results were analyzed using paired T-tests. Secondary measures of our study were assessed by survey and included event reporting knowledge and attitudes.
Conclusions: Data from 41 surveys, including 20 pre- and 21 post-course submissions, were collected from 35% PGY1, 35% PGY2, and 30% PGY3 level residents. Respondents encountered an average of 2.8 events per month and reported these events 25% of the time. The major barriers to reporting included the time required (85%) and the difficulty of using current reporting interfaces (50%). Residents’ ability to correctly identify the key components of the event improved from an average total score of 4.65 to 7.6 (p<0.001) out of a total 10 possible points after the course. The areas of greatest improvement included patient information (p<0.001), staff involved (p<0.001), and the follow-up initiated by the team (p=0.002). Inter-rater agreement on total score was 95.1% with kappa= 0.943 for 41 surveys.In order to learn from our mistakes, the quality of event reporting is critical to support patient safety officers’ review. As information from real-world event reporting is protected and often submitted anonymously, simulated cases are necessary to assess the quality of reporting by providers. Preliminary data shows that residents were able to apply these concepts to the practice of event reporting. Our next step is to offer this session to all internal medicine residents at our institution, and we ultimately aim to teach this module to our medical students as well.