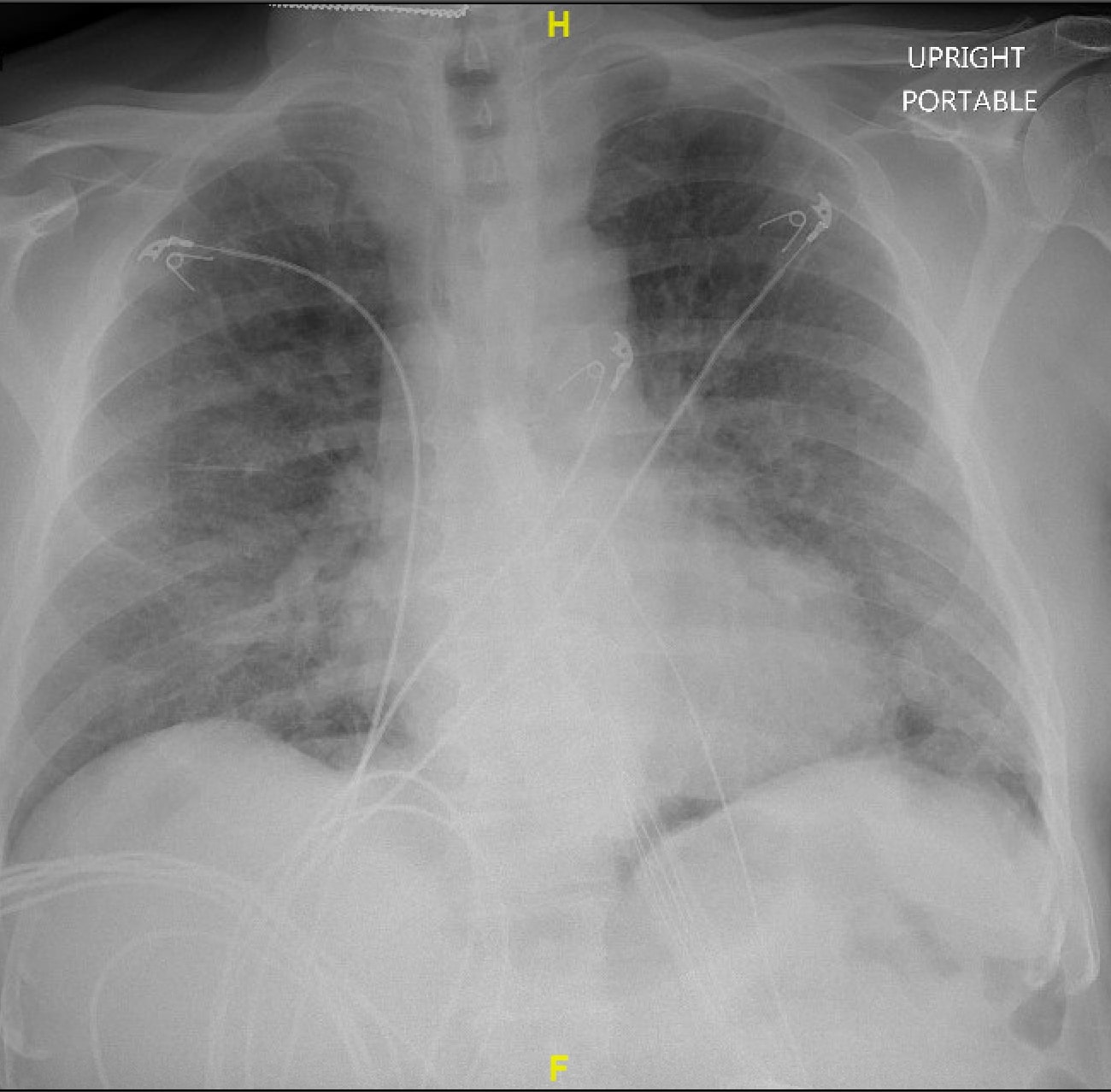
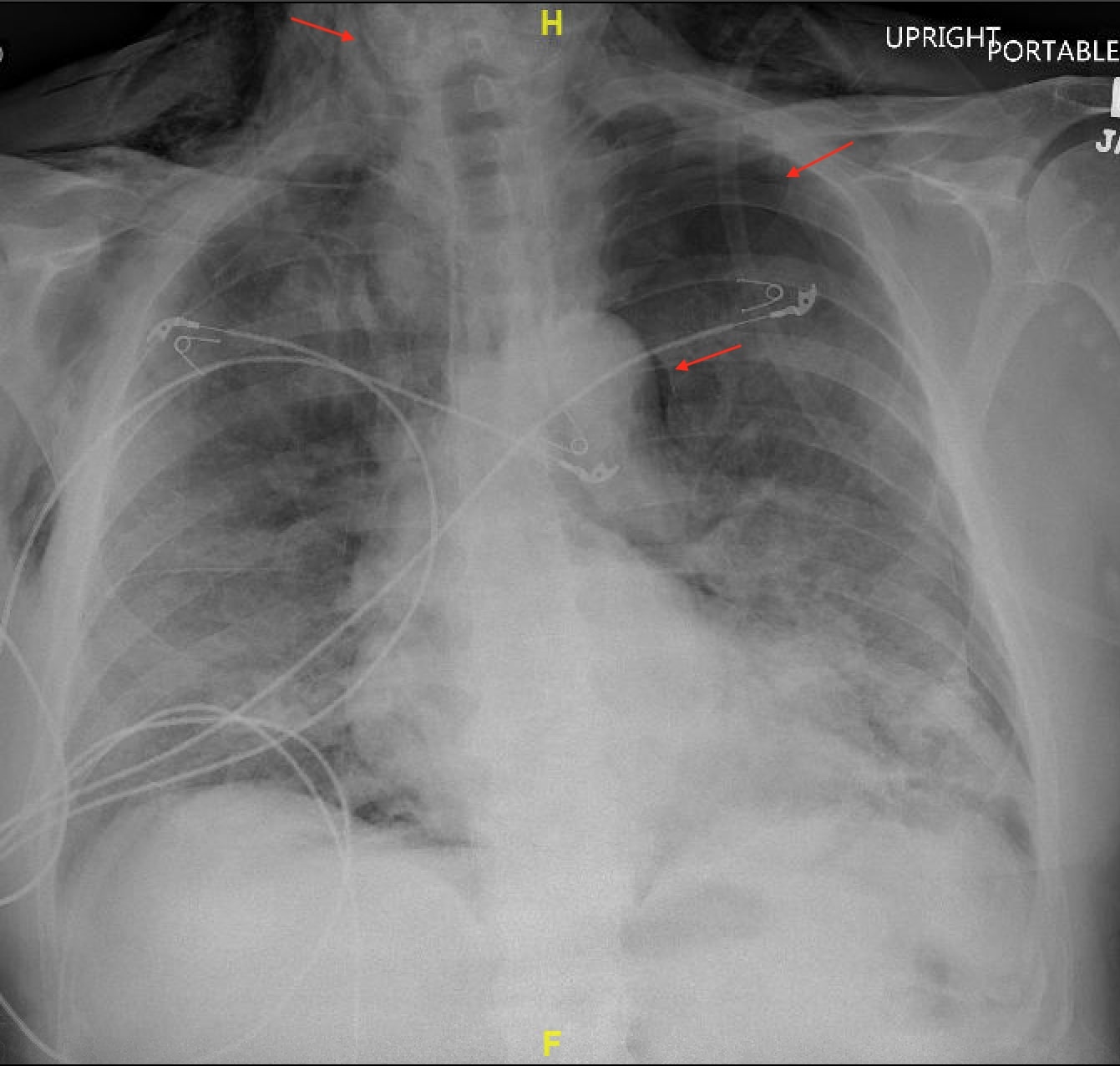
Case Presentation: A male in his 70s with a history of paroxysmal atrial fibrillation presented to the hospital for evaluation of shortness of breath, dysgeusia, and subjective fever. His home medications were aspirin, atorvastatin, pantoprazole, apixaban, and tramadol. Physical exam on admission revealed bilaterally diminished breath sounds in addition to being tachypneic and hypoxic. His ferritin, CRP and d dimer were 2721ng/ml, 206mg/L and 1,332ng/ml. The respiratory viral panel was positive for SARS-CoV2. X-ray imaging revealed multifocal airspace opacities suggestive of COVID-19 pneumonia (figure 1). CT scan of the chest revealed diffuse bilateral groundglass airspace disease with no evidence of pulmonary embolism. He was placed on 10 L /min of oxygen through high flow nasal cannula. He received Dexamethasone, Remdesivir, and was enrolled in a Monoclonal Antibody study. In view of concern for presumed bacterial infection, he was also started on ceftriaxone and azithromycin. On day 2, his oxygen requirements continued to worsen, and was placed on 50 L/min of 100% FiO2. His CRP and d dimer increased to 211.97mg/L and 5,536ng/ml. He was started on a therapeutic dose of enoxaparin in place of apixaban. He was started on Bilevel positive airway pressure ventilation (BiPap) with inspiratory IPAP of 10cm H20 and expiratory EPAP of 8cm H20 at night-time. On day 3, he started complaining of acute, severe, bandlike chest pain. Physical exam revealed crepitus in his neck. He was saturating 88% on Bipap. X-ray imaging revealed new bilateral pneumothoraces, pneumomediastinum with subcutaneous emphysema (figure 2). Surgical service was consulted, and he had thoracostomy and bilateral chest tube placement. In view of persistent hypoxia despite maximum non-invasive ventilatory therapy, goals of care conversation were held with the patient and his family. The patient did not want further escalation of care and was transitioned to inpatient hospice. He died the following day.
Discussion: Pneumothorax can be categorized as primary, secondary, spontaneous, traumatic, or iatrogenic in etiology. The development of pneumothorax is most closely associated with pre-existing lung conditions and the presence of bullae or pneumatoceles. Spontaneous pneumothorax and pneumomediastinum have been described previously in COVID-19 patients. [1-5] Positive airway pressure therapy has been previously associated with spontaneous pneumothorax.[6] There was one previous report of a COVID-19 patient who developed pneumothorax after being placed on High flow nasal cannula, although pneumothorax was felt to be more likely due to COVID-19 pneumonia.[7] Our patient did not have any pre-existing lung conditions, history of tobacco use, or presence of pneumatoceles that would have facilitated the occurrence of this complication. Postulated mechanisms of pneumothorax and pneumomediastinum in COVID-19 could be related to increased alveolar pressure and diffuse alveolar injury along with low compliance that makes the alveoli more prone to rupture, causing free air to track along mediastinal structures.
Conclusions: The co-occurrence of pneumothorax and pneumomediastinum is rare in COVID-19 patients. Prompt recognition of early signs and symptoms of pneumothorax and pneumomediastinum in COVID-19 patients is necessary to minimize morbidity and mortality. The use of minimum amounts of Positive Pressure Ventilation to achieve acceptable tissue oxygenation may reduce the incidence of pneumothorax and pneumomediastinum.