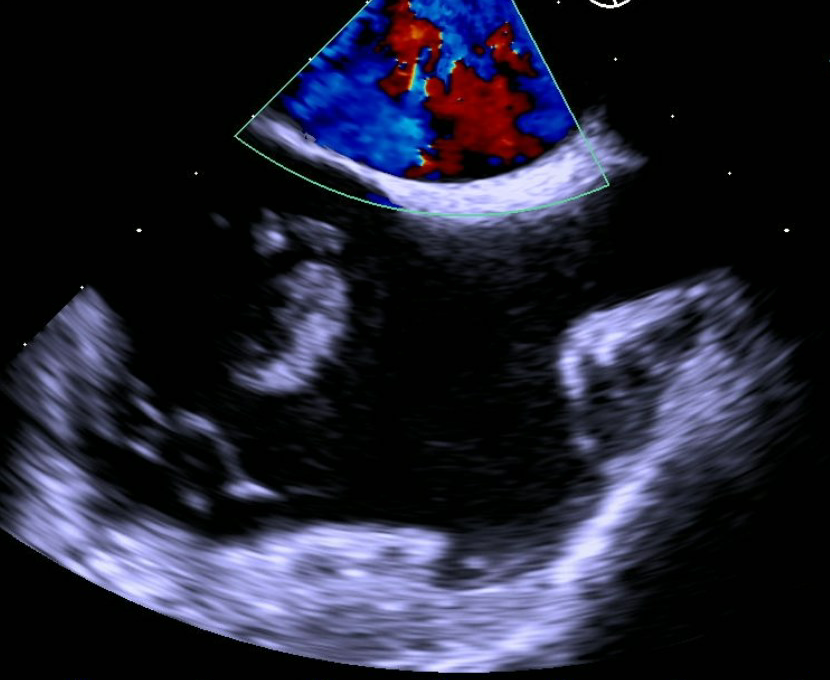
Case Presentation: A 28-year-old female with a PMH of intravenous drug use (IVDA) and untreated hepatitis C presented to the ED with one-week history of painful, erythematous, and tender skin in both upper and lower extremities. She also endorsed myalgia, pleuritic chest pain, and last use of heroin the day prior. She denied fever or SOB. In the ED, her vitals were BP 141/71, HR 146, RR 18, O2 99% on RA and T 98.3°F. The examination revealed multiple track marks on the upper extremities and multiple erythematous, tender, demarcated areas located in the right upper extremity, left wrist, right thigh, and bilateral ankles. Additionally, a systolic murmur along the left lower sternal border was noted, as were decreased breath sounds, greater on the right side. Laboratory studies revealed WBC 17.35 (bandemia15%), lactic acid 2.5, AST 75, ALT 114, and Hepatitis C RNA 662,000. A CT chest without contrast revealed bilateral pulmonary cavitary nodules, likely septic emboli, a moderate right pneumothorax (20-25%) and a small right pleural effusion. The patient was admitted for sepsis secondary to cellulitis with possible endocarditis and started on broad spectrum antibiotics. The pneumothorax was managed conservatively with supplemental oxygen. An initial TTE revealed a large pedunculated echogenic mass (25mm x 3mm) in the right atrium which appeared to be attached to the free wall, separate from the tricuspid valve; blood cultures grew MRSA. A subsequent TEE revealed a 2.7cm mobile, linear echo density in the right atrium, attached to the right atrial wall, likely an infected thrombus. Cardiothoracic surgery recommended medical management, including anticoagulation, without surgical intervention. A follow-up chest x-ray demonstrated resolution of the pneumothorax. The endocarditis and cellulitis improved with antibiotics. Hospital course was complicated by development of R posterior thigh abscess that required drainage. The remainder of the hospitalization was unremarkable, and the patient completed a six-week course of antibiotics.
Discussion: Infective endocarditis (IE) commonly occurs in patients who use intravenous drugs. However, spontaneous PTX is a rare complication of IE. Spontaneous PTX from right-sided endocarditis was first reported in the literature by Aguado, et al in 1990. Since then, less than a dozen case reports have been reported with patients who have developed pneumothoraxes as complications of endocarditis. Typical symptoms of pneumothorax include shortness of breath, chest pain, chest tightness. Exam findings can demonstrate decreased breath sounds. Diagnosis of a pneumothorax is made via chest x-ray/CT chest. Treatment can include chest tube drainage or conservative management via serial chest x-rays. Also, unique to our case is that our patient had non-valvular IE; IV drug users have higher rates of right-sided valvular endocarditis. IE diagnosis is made via positive blood cultures and vegetations on echocardiography. Surgical intervention is recommended in those that have severe valvular regurgitation, abscesses, heart failure. Antimicrobial treatment is targeted toward the bacterium and can last at least six weeks from negative blood cultures.
Conclusions: Physicians should keep PTX in the differential for IVDU patients presenting with acute shortness of breath.