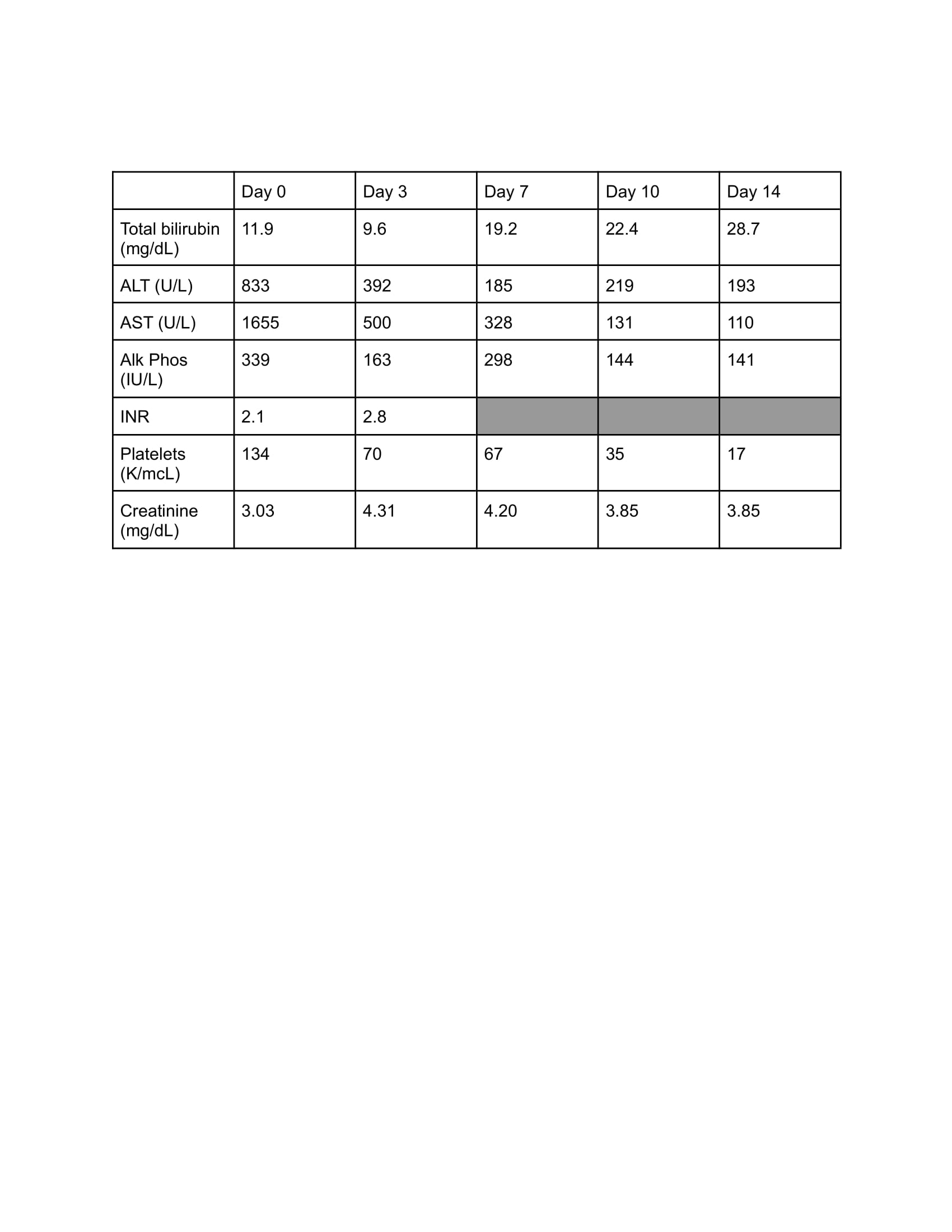
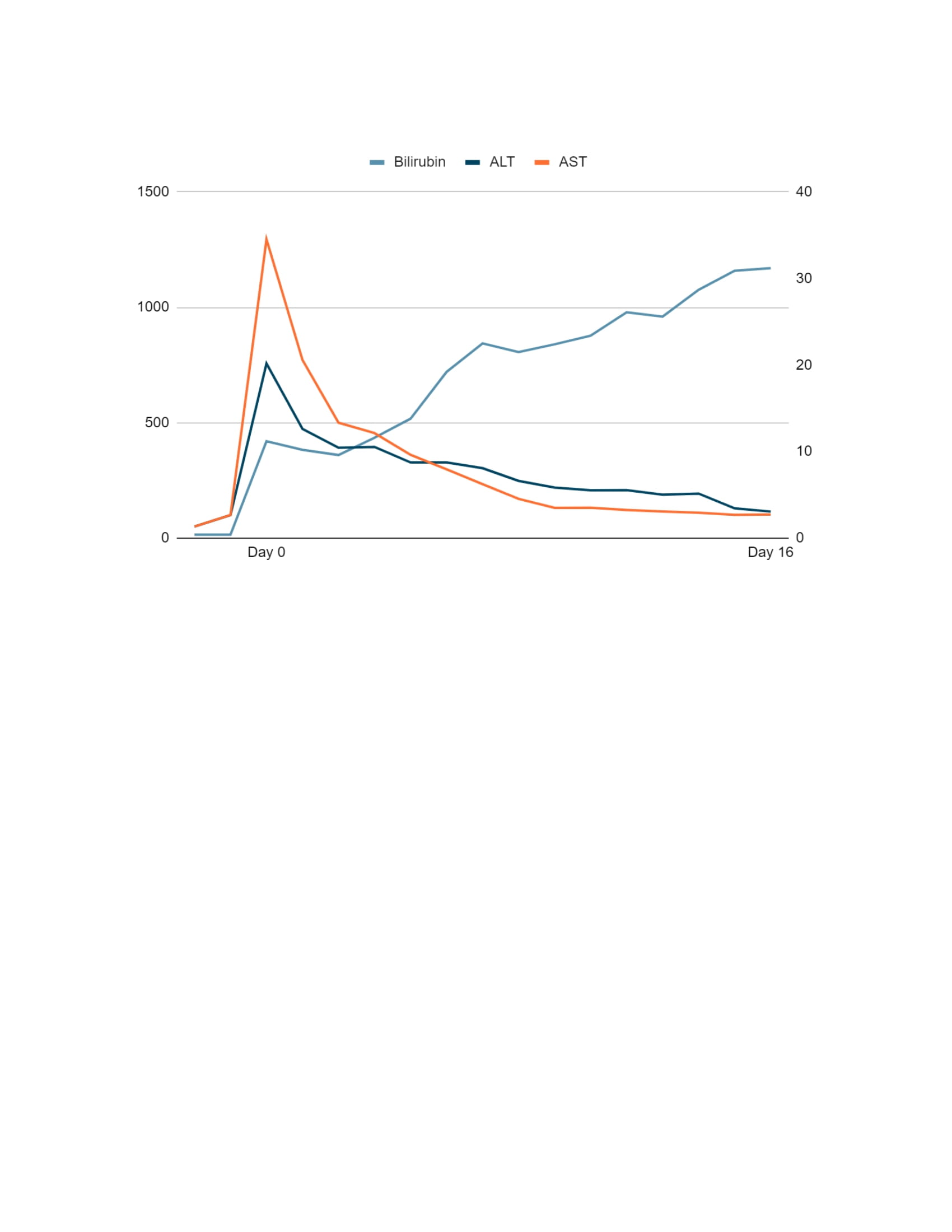
Case Presentation: 54 year-old female with past medical history of stage IV right renal cell carcinoma s/p nephrectomy and recurrent urinary tract infections secondary to left staghorn calculus was admitted for generalized weakness, fatigue, nausea, vomiting and altered mental status. Physical exam showed scleral icterus. Lab work was significant for elevated aminotransferases, bilirubin and alkaline phosphatase in a mixed hepatocellular/cholestatic pattern. Other pertinent abnormalities included hyperammonemia, elevated creatinine and INR, hypoalbuminemia, and thrombocytopenia. Abdominal ultrasound showed a nodular liver, large ascites and patent portal vein with normal directional flow. CT abdomen showed a normal spleen and a large staghorn calculus in the left kidney without hydronephrosis. Autoimmune workup with ANA, anti-smooth muscle antibody, anti-LKM 1 antibody, antimitochondrial antibody and immunoglobulins were normal. Salicylate and acetaminophen levels were normal. Acute and chronic viral hepatitis panels were negative. Ascitic fluid analysis didn’t show evidence of SBP. Medication reconciliation showed that the patient was prescribed nitrofurantoin 100 mg twice daily for E. coli urinary tract infection about 10 days prior. Patient was treated for hepatic encephalopathy and hepatorenal syndrome along with empiric course of steroids for presumed DILI secondary to nitrofurantoin. During hospital course patient didn’t show any clinical or biochemical evidence of recovery with worsening mentation and was ultimately upgraded to ICU requiring intubation. She was eventually transitioned to comfort care and extubated palliatively. Liver function tests during hospital course are shown in Figure/Table 1.
Discussion: Nitrofurantoin is one of several first-line antibiotics commonly prescribed for uncomplicated urinary tract infections. We present a rare case of acute drug-induced liver injury (DILI) secondary to nitrofurantoin with fatal outcome. Nitrofurantoin-induced liver injury can present as acute or chronic hepatitis-like syndrome. The acute form is extremely rare at 0.3 cases per 100,000 prescriptions and usually presents after a 1 to 2 week course of treatment. Severity of presentation ranges from mild transaminitis to fulminant hepatic failure and death. Rapid recovery is typically expected after stopping the offending drug. Pathogenesis is not completely understood however nitrofurantoin hepatotoxicity shares many features of autoimmune hepatitis and in severe cases corticosteroids are used. Our patient didn’t show any recovery with discontinuation of nitrofurantoin as well as steroids and was not a candidate for liver transplantation given history of renal cell carcinoma. Other proposed treatments such as N-acetylcysteine have unproven benefit.
Conclusions: Clinicians should have a clinical suspicion for DILI in patients presenting with acute liver injury. Preventative measures for patients taking hepatotoxic agents are not well studied but may include monitoring of aminotransferases during active use, however frequency of monitoring and the level of transaminitis for discontinuation of offending drug remains controversial.This case report highlights importance of short term fatal hepatotoxic effects of nitrofurantoin for physician awareness and encourages further research to formulate guidelines for management to help decrease mortality.