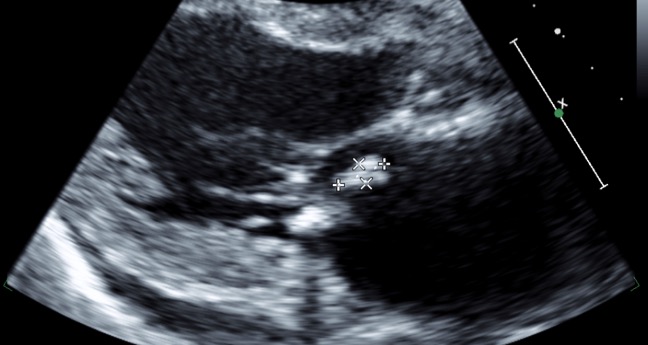
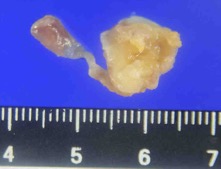
Case Presentation: A 78-year-old Japanese man with chronic heart failure and type 2 diabetes presented with a 2-day history of recurrent fever six days after the termination of a 12-day antimicrobial treatment for pyelonephritis caused by Escherichia coli. The physical examination revealed a body temperature of 38.9 °C, respiratory rate of 24 breaths per minute, and tenderness at the prostate gland. Blood culture results upon admission revealed the presence of E. coli. Furthermore, vegetation (measuring 4.3×18 mm diameter) was detected using a transthoracic echocardiogram on the mitral posterior leaflet (Figure 1), which was confirmed by transesophageal echocardiogram. E. coli was further recovered from blood culture twice on separate days. We diagnosed the patient with infective endocarditis caused by E. coli. The vegetation was removed and mitral valvuloplasty was performed seven days after admission (Figure 2). The patient received antimicrobial drugs intravenously (ceftriaxone plus gentamicin to ceftriaxone plus ciprofloxacin) for a total of 6 weeks. Despite an episode of bilateral acute multiple cerebral infraction which occurred due to the endocarditis, the patient fully recovered from the infection.
Discussion: Only 1.8% of the endocarditis cases are caused by non-HACEK gram-negative bacilli, being predominantly associated with implanted endovascular devices. A history of heart disease, diabetes, and older age are all risk factors for non-HACEK gram-negative bacillus endocarditis. If the clinical course of patients presenting with gram-negative bacillus bacteremia is unusual, it is important to consider endocarditis in addition to abscesses to achieve an early diagnosis. The in-hospital mortality rate of non-HACEK gram-negative bacillus endocarditis is higher (24%) than that of other bacterial endocarditis (17%), which is thought to occur due to a delay in diagnosis. The time from onset to diagnosis of non-HACEK gram-negative bacillus endocarditis was predominantly reported to be more than one month; however, in this case, the time from onset and relapse to diagnosis were 25 days and 7 days, respectively. We believe that this earlier diagnosis might have contributed to the good clinical outcome. Furthermore, surgical intervention is associated with a favorable outcome in patients with non-HACEK gram-negative bacillus endocarditis. Hence, we believe that aggressive surgical intervention might have also contributed to the favorable clinical course.
Conclusions: Here, we report the case of a surviving older patient presenting with endocarditis caused by E. coli. The disease was diagnosed early by hospitalists, and the patient benefited from a rapid examination by cardiologists, treatment support by infectious disease physicians, and aggressive intervention by cardiovascular surgeons. We advocate that an early diagnosis and aggressive surgical intervention are paramount to achieving a good clinical outcome in patients with (otherwise fatal) non-HACEK gram-negative bacillus endocarditis.