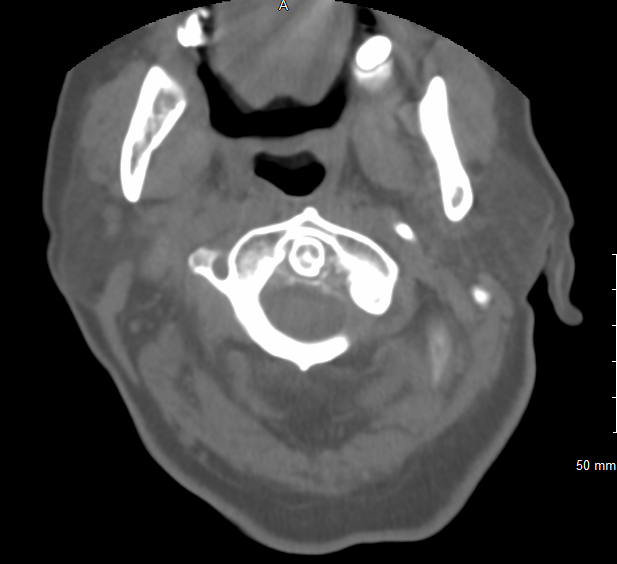
Case Presentation: A 71-year-old woman with a past medical history of hypertension, hyperlipidemia, and osteoarthritis presented with four days of fevers, intermittent confusion, subjective weakness, and pain in the neck and left shoulder. On examination, she exhibited tenderness to palpation of the neck with significantly limited rotational range of motion. The left shoulder was also tender to palpation with range of motion limited by pain. Vital signs were notable for temperature of 101.7F. Laboratory examination showed white blood cell (WBC) count of 25 with neutrophilic predominance, erythrocyte sedimentation rate (ESR) of 125, and C-reactive protein (CRP) of 480. The patient was started on empiric antibiotics given her fever and leukocytosis. A CT scan of the cervical spine demonstrated chondrocalcinosis of the atlantoaxial joint (Figures 1, 2), and her subsequent MRI of the cervical spine showed diffuse edema with ill-defined enhancement of the upper paraspinal muscles extending from the suboccipital soft tissues to the C6-C7 level without evidence of osteomyelitis, discitis, or spinal epidural abscess. As no infectious source was identified, antibiotics were discontinued on hospital day 3. On hospital day 4, rheumatology consult noted that the clinical presentation was consistent with a diagnosis of Crowned Dens Syndrome, and empiric treatment with ibuprofen 600mg every eight hours was initiated. By hospital day 6, the patient showed significant improvement in pain and range of motion in the affected joints as well as normalization of her WBC, ESR, and CRP. She was discharged home on hospital day 8 at her functional baseline.
Discussion: Crowned Dens Syndrome is a rheumatologic process in the family of calcium pyrophosphate crystal deposition (CPPD) diseases. Deposition of calcium pyrophosphate or hydroxyapatite crystals in the synovial membrane, articular capsule, and various ligaments surrounding the dens causes acute inflammation that manifests clinically as neck pain and stiffness, commonly with restriction in rotational range of motion of the neck. Patients may also present with headache, meningism, or cervico-brachial pain. Evidence of systemic inflammation, such as fever, leukocytosis, and elevated ESR and CRP, is common. CT scan of the cervical spine is the technique of choice for identifying the presence of calcium deposition surrounding the dens, though the finding is non-specific and must be clinically correlated to make the diagnosis. The disease has a good prognosis, generally self-resolving within several weeks without chronic sequelae; non-steroidal anti-inflammatory drugs (NSAIDs) or colchicine can be used to expedite resolution of symptoms.
Conclusions: Crowned Dens Syndrome should be considered in the differential diagnosis for patients presenting with acute neck pain and stiffness, headache, fever, leukocytosis, and elevated inflammatory markers. Due to its similarity with infectious and other rheumatologic disorders, patients may receive unnecessary diagnostic and therapeutic interventions including systemic antibiotics, steroids, lumbar puncture, or temporal artery biopsy. Early consideration of a diagnosis of Crowned Dens Syndrome with appropriate radiologic correlation may help to reduce morbidity associated with unnecessary interventions and delayed diagnosis.