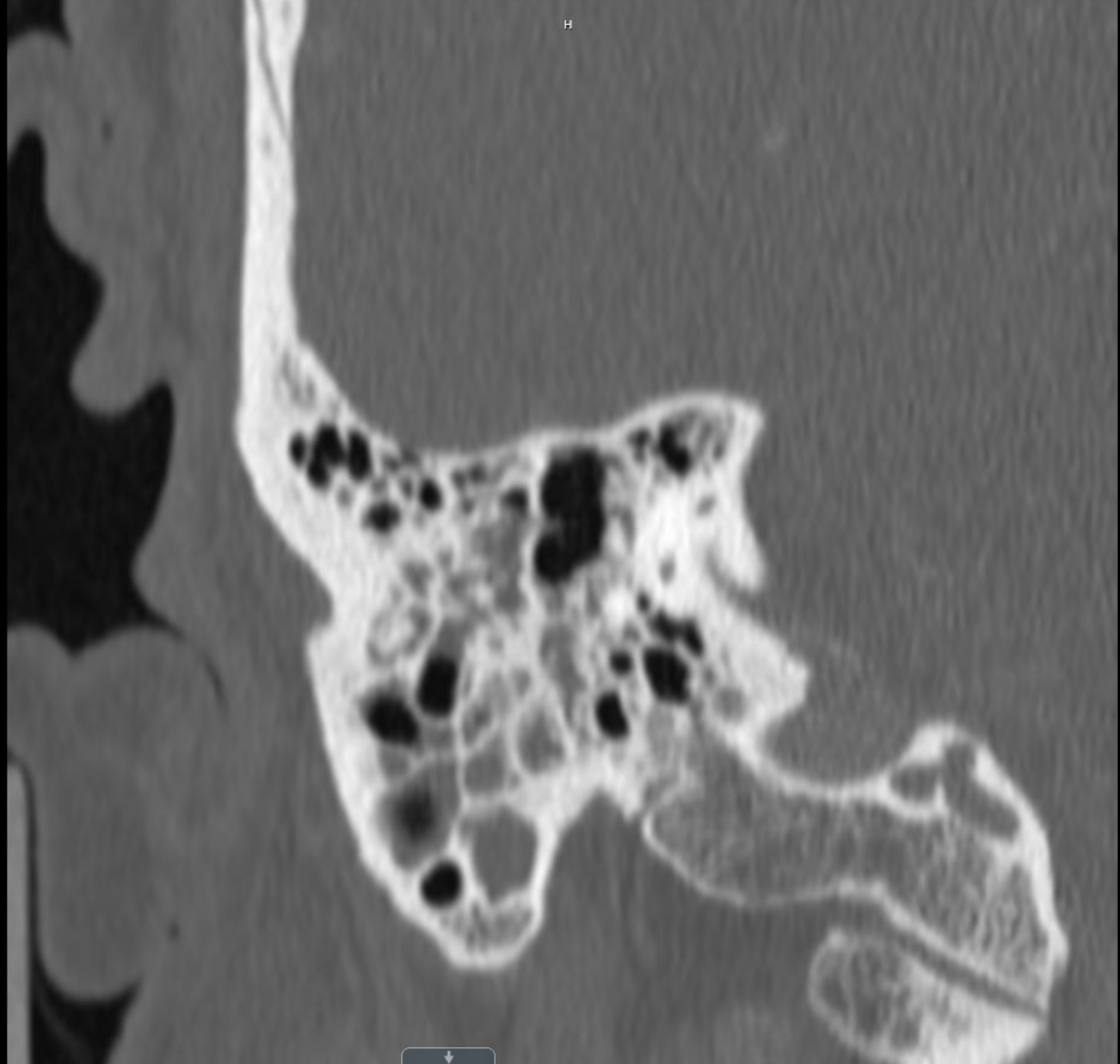
Case Presentation: A 64 year-old Caucasian man with a history of atrial-flutter and hypertension presented with nasal congestion, eye redness, headaches, and progressive hearing loss over 8 months. His longstanding partial left-sided hearing loss progressed to complete hearing loss. In addition, he developed a new right-sided hearing loss. He also complained of right-sided Bell’s Palsy, dysgeusia and 20-pound weight loss.He was previously treated for recurrent sinusitis and persistent headaches with several courses of antibiotics without improvement. He was also prescribed prednisone, which provided temporary relief from his headaches, but no improvement in hearing loss. Prior evaluation by community ENT and ophthalmology did not yield a clear diagnosis. However, imaging findings suggested mastoiditis, so he was treated with another course of antibiotics. Because his symptoms persisted, he presented to our emergency department.Examination showed bilateral conjunctival injection, mild right eyelid ptosis, weak left eyelid closure, and full visual fields. Hearing was diminished on the right and markedly reduced on the left. External ear canals were patent bilaterally with the left tympanic membrane appearing erythematous and bulging. Mastoid processes were non-tender.Laboratory tests showed WBC of 13.7, ESR of 107, and CRP of 19. Autoimmune workup revealed positive p-ANCA with 1:80 titer, positive myeloperoxidase antibody, and elevated RF of 28. Other studies, including ANA, proteinase 3 antibody, CCP antibody, RPR, hepatitis serologies, and HIV were all negative.Brain MRI revealed asymmetric dural enhancement over the L temporal lobe and L>R mastoid air fluid signal. CSF had elevated protein of 106 but was otherwise normal. Chest CT was negative for sarcoidosis or malignancy. CT of the temporal bones showed progressive opacification of bilateral mastoid air cells and middle ear cavities, as well as enlargement of the right lacrimal gland. Tympanostomy showed no fluid but granulation tissue was noted. Finally, lacrimal gland biopsy was consistent with IgG4-related chronic dacryoadenitis. Serum IgG subclass 4 concentration was not elevated.The patient was treated with methylprednisolone 500 mg IV daily for 3 days and was started on rituximab.
Discussion: IgG4-Related Disease (IgG4-RD) is an emerging immune-mediated fibroinflammatory disease that often mimics other conditions and has been described as affecting the eyes, ears, sinuses, and meninges. Although considered a rare condition, its true prevalence is unknown as it has not been widely recognized and does not even have an assigned unique international diagnostic code. It is likely substantially misdiagnosed and underreported. Clinical manifestations often result from subacute progressive growth within an organ or the development of diffuse organomegaly. We report a case of IgG4-RD mimicking mastoiditis and resulting in cranial nerve VII and VIII palsies.Histopathology is the mainstay in diagnosis of IgG4-RD. Elevated concentrations of IgG4 in tissue and serum are helpful but neither one is a specific diagnostic marker in IgG4-RD. Treatment consists of steroids and immunosuppressants, which have previously been shown to restore cranial nerve function.
Conclusions: IgG4-RD is a rare fibroinflammatory disease that is increasingly being recognized. It must be considered in patients presenting with subacute progressive and persistent mastoiditis of unclear etiology.