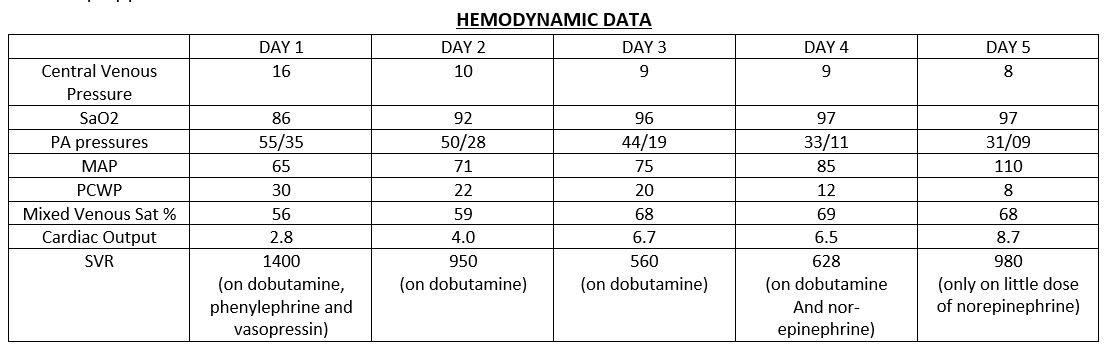
Case Presentation: 56-year-old female presented to ED with a two-week history of fever, chills, headache, intermittent nausea and vomiting, mild abdominal pain. Her comorbidities included Diabetes mellitus, Morbid obesity, and Hypertension. She had mild leukocytosis on complete blood count and had physical examination significant for bilateral rhonchi in chest auscultation. She was admitted under the impression of community-acquired pneumonia and pneumonia workup was sent. She was started on broad-spectrum antibiotics, but later decompensated and was intubated for severe hypoxic respiratory failure, and suspect ARDS. She soon went into shock requiring multiple vasoactive medications. Her antibiotic coverage was broadened further to include vancomycin, piperacillin-tazobactam, azithromycin, and oseltamivir. Her Troponin and D-Dimer levels were elevated with minimal changes in EKG. BNP was >50000. ECHO showed 39% Ejection Fraction and inferolateral wall motion abnormalities. She was started on low dose dobutamine for inotropic support. ESR and CRP were significantly elevated. Due to multiple factors in presenting history and lab test reports, she was suspected to have myocarditis. A right heart catheterization revealed elevated right and left heart filling pressures. The patient was started on Furosemide therapy. With diuresis and dobutamine, her ventilator requirements improved considerably. Her Urine Legionella antigen came back positive on day 3 for which she was continued on azithromycin. Impression was changed to Legionella Myocarditis. With continued improvement, she was successfully weaned off the ventilator on day 7 and transferred to the medical floor. A repeat echocardiogram revealed complete normalization of wall-motion abnormalities seen earlier. She was discharged home with 14-day course of azithromycin.
Discussion: Legionnaires Disease is a systemic illness caused by Legionella Pneumophilla. It is an important but relatively uncommon respiratory infection that can cause substantial morbidity and mortality. This is most commonly caused by Legionella Pneumophilla. Transmission of Legionnaires’ disease is usually by inhalation of aerosols or aspiration of water containing Legionella spp; no evidence of person-to-person transmission exists. Legionella Pneumophilla usually causes respiratory illness, but can rarely involve other systems. Myocarditis is one of the rarest complications of Legionella Pneumophilla, with only around 15 reported cases in PubMed. Treatment for legionella is by macrolides if the infection is not severe, and with combination therapy in severe infection. Macrolides are combined with either a quinolone or rifampicin.
Conclusions: In conclusion, our case signifies that legionella infection should be suspected in patients who present with community-acquired pneumonia, with extra-pulmonary involvement, especially cardiac. A high clinical suspicion is essential for diagnosis. Early diagnosis and treatment of legionnaires disease may be life-saving.