Case Presentation:
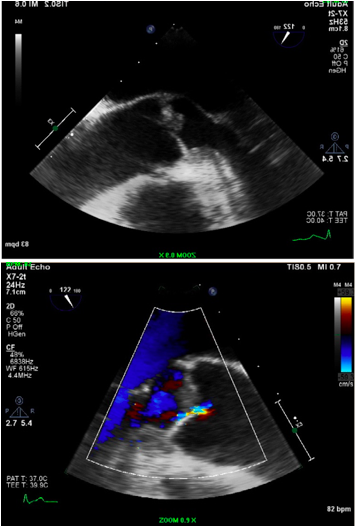
A 62 year old male with past medical history of DVT, prostate cancer diagnosed 2 years ago, presented to the hospital complaining of 1 day weakness in his left upper and lower extremities. Head CT revealed a sub-acute right side ischemic infarct. Physical exam was significant for jaundice, left facial droop, left tongue deviation and a strength of 3/5 in Left upper/lower extremity. Laboratory findings were significant for elevated liver enzymes. MRI of the brain confirmed the ischemic nature of the stroke. TEE showed a large mass 7mm x 6mm on the left ventricular surface on the non-coronary cusp of the aortic valve. Six Sets of blood cultures were drawn and empiric broad-spectrum antibiotics were initiated. On day 5, all blood cultures were negative and antibiotics were discontinued. Given the lack of fever and the history of malignancy, the diagnosis of “Non-bacterial thrombotic endocarditis” (NBTE) was made. Oncology service was consulted because of the history of untreated prostate cancer. A total body Bone scan and a chest CT were negative. Abdominal MRI showed a Large infiltrating liver mass. An IR guided biopsy of the liver mass was obtained and the pathology report revealed metastatic prostate adenocarcinoma. After a multidisciplinary discussion between internal medicine, infectious disease, oncology and CT surgery, the decision was against surgical management of the large aortic vegetation given the overall poor prognosis of the metastatic prostate cancer. Patient was treated with systemic anticoagulation.
Discussion:
NBTE is a rare condition that is most commonly seen in advanced malignancy. NBTE is often an autopsy finding. However, some patients are diagnosed antemortem presenting with the signs and/or symptoms of systemic embolization and require therapy. There are no laboratory tests that confirm the diagnosis of NBTE. Typically, at least three sets of blood cultures should be taken prior to any empiric antibiotic therapy. The absence of the typical organisms that cause culture-positive endocarditis and atypical organisms that cause culture-negative endocarditis help support the diagnosis of NBTE. A TEE is needed if a TTE is non-diagnositic.
Therapeutic dose of subcutaneous low molecular weight (LMW) heparin or intravenous unfractionated heparin should be used, rather than warfarin or a direct thrombin or factor Xa inhibitor. Anticoagulation should be continued indefinitely, since recurrent thromboembolism has occurred in patients following its discontinuation.
Conclusions:
NBTE is a rare condition. Patients are typically asymptomatic until embolization occurs. The workup includes an echocardiogram and defining the underlying cause. Treatment consists of systemic anticoagulation and therapy directed at treating the underlying malignancy or associated condition. Surgery is rarely performed. Despite therapy the prognosis from NBTE is generally poor.