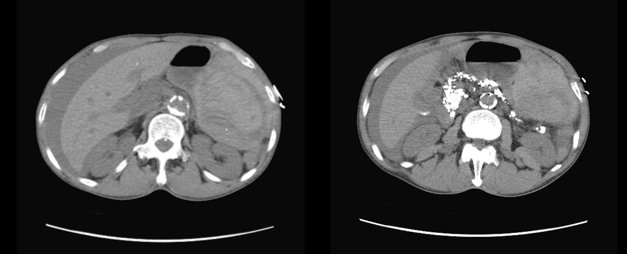
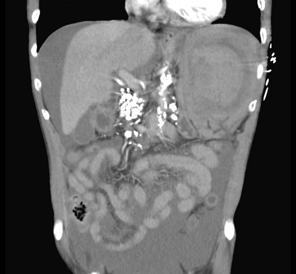
Case Presentation: A 56 year-old male with past medical history of chronic pancreatitis, alcoholic cirrhosis, cured hepatitis C, iron deficiency anemia and gastric arterio-venous malformations (AVM) status post cauterization presented for screening colonoscopy and esophagogastroduodenoscopy (EGD). EGD showed several nonbleeding gastric AVM status post Argon Plasma Coagulation. The colonoscopy was unremarkable without any reported difficulty and the patient was discharged home. The following evening he presented to the emergency department with diffuse abdominal pain that was associated with dizziness, four episodes of bilious non-bloody vomiting and non-bloody diarrhea. On exam, blood pressure (BP) was 80/40 but other vitals were normal. His abdomen was diffusely tender to palpation with hypoactive bowel sounds and rectal exam was normal with brown stool and no signs of bleeding. Labs were pertinent for severe anemia with hemoglobin of 6.1 g/dl which dropped from the day prior (10.1 g/dl), acute kidney injury with creatinine of 2 (0.8 day prior) and anion gap acidosis with a lactate level of 15. Abdominal X-ray was unremarkable. CT Abdomen/Pelvis revealed large amount of free fluid and hemoperitoneum in the left upper quadrant with presence of splenic remnant with a focal area of high attenuation suggestive of active contrast extravasation (Fig 1-3). He was immediately taken to the operating room and was found to have a ruptured spleen with hemoperitoneum. The spleen was removed, and hemostasis was achieved. After the procedure, his vitals were stable and his abdominal pain improved with no further bleeding.
Discussion: Splenic rupture after colonoscopy is a rare complication, with an incidence of approximately one case per 100,000 colonoscopies (1). The first case was published in 1974 (2). The mechanism is thought to be from direct trauma while passing the endoscope through the splenic flexure, avulsion of the splenic capsule by excessive traction on the splenocolic ligament, or from traction on preexisting adhesions located between the colon and spleen (3, 4, and 5). However, studies directed to understand the exact mechanism have yet to be completed. Risk factors for splenic injury post colonoscopy (6) include a history of abdominal surgery or trauma that have led to splenocolic adhesions, hematological, infectious and infiltrative diseases with associated splenomegaly, inflammatory bowel disease, and pancreatitis (which our patient had a history of). Having said that, splenic injuries can and have occurred in patients without any risk factors and who had reportedly easy colonoscopies.Signs and symptoms may include abdominal pain, left shoulder pain, and orthostatic changes. Diagnosis is made by abdominal CT (5). Management is usually with splenectomy. However, clinical observation and conservative management is an alternative approach if the patient is hemodynamically stable (6).
Conclusions: Colonoscopy is a very common procedure. It was estimated that approximately 14.2 million colonoscopies have been performed in 2002 (7). Hemorrhage, infection, perforation, hypotension, and aspiration are all well-known colonoscopy complications. However, post colonoscopy splenic rupture is rare. Physicians need to consider this in the differential diagnosis of post colonoscopy abdominal pain.