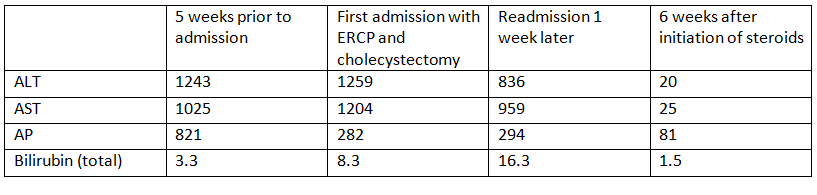
Case Presentation: A 70-year-old woman was admitted to our medical center with a 2-month history of abdominal discomfort, anorexia and fatigue. Past medical history was notable for hyperlipidemia. Five weeks prior to admission, the patient presented to her primary provider with similar complaints and was found to have significantly elevated liver enzymes, as shown in Table 1. The patient denied alcohol use. At the time of admission, work-up showed similar transaminases with an increase in bilirubin (Table 1). Abdominal ultrasound revealed cholecystolithiasis and possible cholecystitis without intra- or extrahepatic ductal dilation. ERCP confirmed cholecystolithiasis without visualization of intraductal stones on cholangiogram or after sweeping of the biliary tree. Laparoscopic cholecystectomy was performed and pathology results revealed chronic cholecystitis. Despite these interventions, the patient was readmitted one week later for ongoing jaundice and malaise. She had no ascites on exam. Laboratory work-up showed persistently elevated liver tests (Table 1). Anti-smooth muscle antibodies (ASMA) were elevated at 1:80. Viral hepatitis panel was negative. Liver biopsy revealed marked panacinar hepatitis with cholestasis without hemosiderin deposition. The patient was diagnosed with autoimmune hepatitis and initiated on steroids with rapid resolution of symptoms. Transaminases and bilirubin decreased significantly one week after initiation of steroids and normalized after 6 weeks.
Discussion: The clinical presentation of autoimmune hepatitis (AIH) is often nonspecific and highly variable. Most patients present with insidious symptoms, but the spectrum of symptomatology can range from asymptomatic to severe acute disease. Although initial reports have suggested that AIH has a bimodal age distribution (with the second peak between 40 and 50 years), the condition has increasingly been recognized in all age groups, including the elderly. Acute AIH can mimic other conditions such as acute viral hepatitis and choledocholithiasis resulting in delayed diagnosis and sometimes unnecessary interventions such as ERCP and cholecystectomy.
Conclusions: In the absence of an obvious alternative diagnosis, acute transaminitis warrants work-up that includes ASMA testing since AIH can present in virtually any age category, as highlighted in this case.