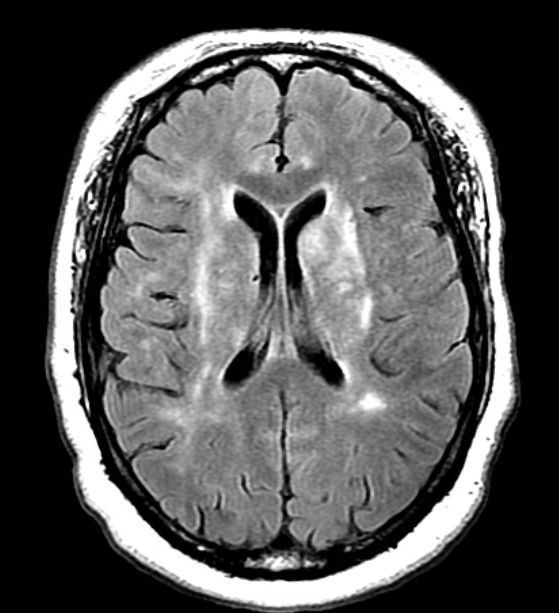
Case Presentation: A 51-year-old African female with 7-year untreated HIV infection presented with sudden-onset acute psychosis. She was agitated and reported auditory hallucinations upon arrival. On exam, she was hemodynamically stable but appeared drowsy, intermittently following one-step commands. She did not have meningismus or focal neurological deficits. Physcial exam of other systems was unremarkable.CBC and CMP revealed lymphopenia and a high protein albumin gap. CT head without contrast showed an ill-defined hypodensity in left basal ganglia. MRI brain with and without contrast showed areas of increased T2 signal intensity in the basal ganglia, thalami, right midbrain, upper pons and white matter. Empirical antibiotics (vancomycin, ampicillin, ceftriaxone, acyclovir) were started for suspected CNS infection. Her HIV-1 antibody was positive with CD4 cell count of 46/uL. A lumbar puncture was performed with normal CSF opening pressure. CSF analysis revealed WBC 15/mL (98% lymphocytes), RBC 1/mL, glucose 56 mg/dl, protein 53 mg/dL, increased IgG and IgG synthetic rate at 16.07 mg/dL, and 38.64 mg/day. CSF cytology was negative for malignancy. Other negative CSF studies included VDRL, cryptococcal antigen, bacterial/fungal stain and culture, AFB, viral PCRs (CMV, HSV, VZV, JC, BK and enterovirus). Qualitative EBV PCR in CSF was positive. EBV serology suggested reactivation. Serum Toxoplasma antibodies and TB T-spot were negative. Given the concern for primary CNS lymphoma, MR spectroscopy was obtained with results suggesting cell death rather than lymphoma.
In the next few days, patient’s mental status deteriorated and progressed to comatose state. Stereotactic brain biopsy was inconclusive. Patient had a cardiac arrest on hospital day 18 and died. Autopsy reported multiple microglial nodules and multinucleated giant cells in basal ganglia, thalamus and brainstem, characteristic of HIV encephalitis. Her CSF 14-3-3, RT QuIC and autoimmune encephalitis panel were later reported negative.
Discussion: This case illustrates a rare presentation of HIV encephalitis in HAART era, with rapid and eventually fatal progression due to years’ untreated HIV infection. HIV encephalitis occurs due to the neuroinflammatory response to HIV penetration into the CNS via transmigration of infected monocytes/macrophages across the BBB. It can present with variable neurological deficits including cognitive and/or motor impairment. Such disease has shifted from a rapidly progressive form to a chronic degenerative process since the introduction of HAART. Focal abnormalities of high signal intensity in basal ganglia, brainstem are commonly seen on MRI for HIV encephalitis. HAART is the treatment for HIV encephalitis.
Although a positive EBV PCR test in CSF is considered a marker for primary CNS lymphoma in HIV/AIDS patients. Recent studies suggest it has been frequently detected in immunocompromised patients as “bystander” in the presence of other infectious pathogens, representing intracerebral EBV reactivation.
Conclusions: Long-time untreated HIV infection can result progressive, fatal HIV encephalitis with imaging findings mimicking primary CNS lymphoma. Clinicians should not rely solely on a positive EBV PCR result in CSF as diagnostic evidence of PCNSL in HIV patients.