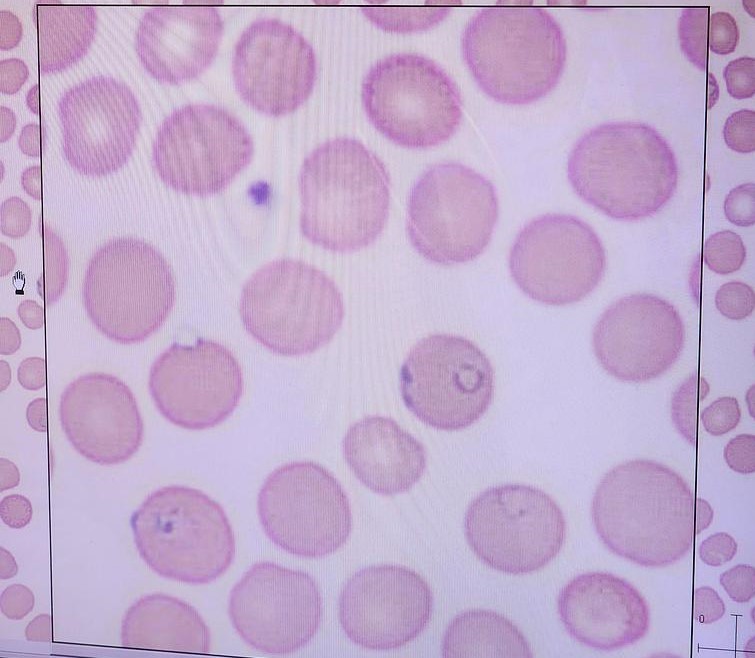
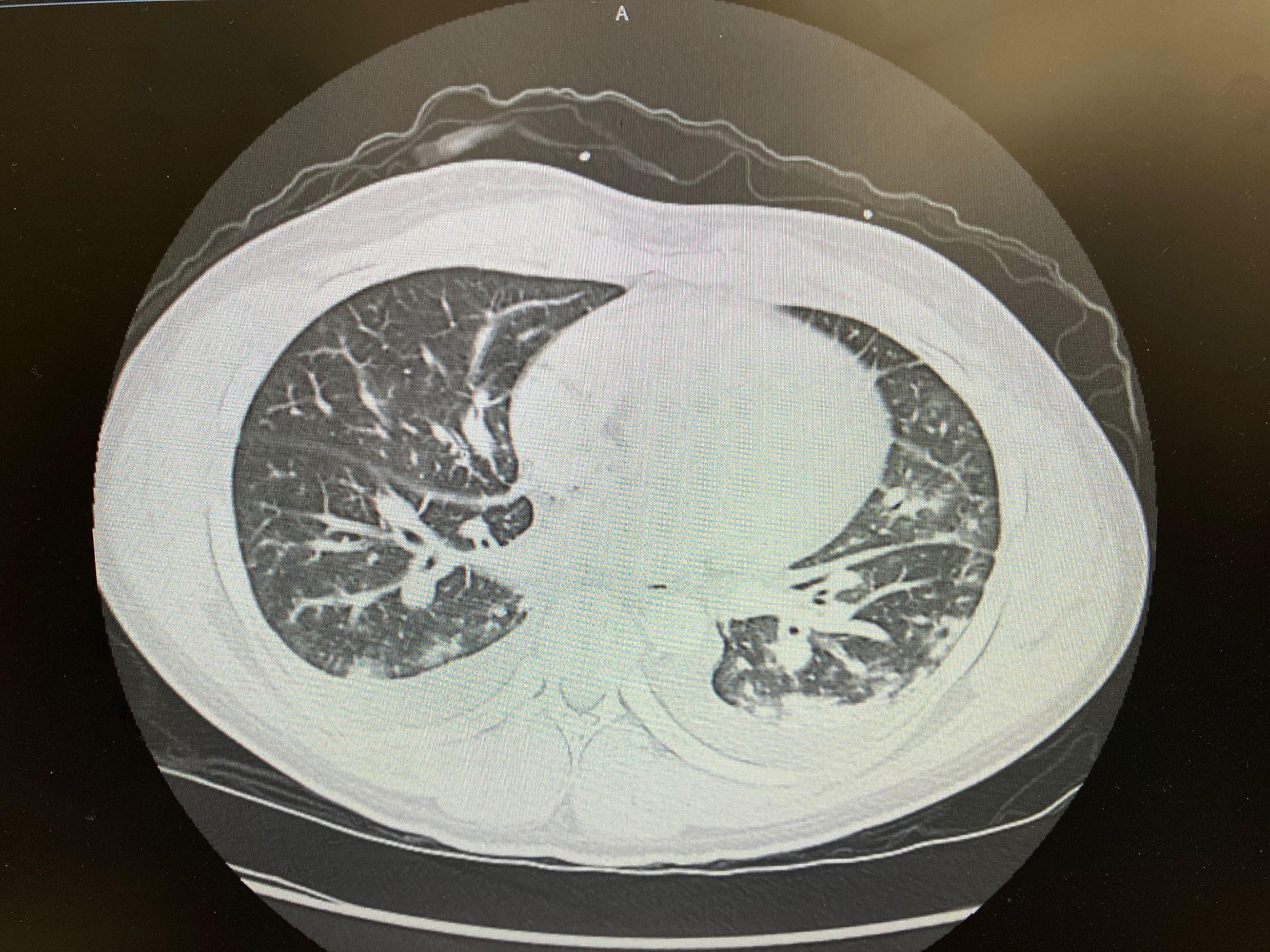
Case Presentation: This is a 32 year old male with no pertinent medical history who presented to the emergency department with complaints of headache, body aches, vomiting, diarrhea, fevers and chills for 4 days. The patient also admits to generalized weakness and poor appetite. The patient denies any chest pain, dyspnea, shortness of breath. The patient does have a recent history of travel to Ghana for a month where he was not consistent with taking his malaria prophylaxis medications. On initial presentation, the patient was febrile to 103 degrees fahrenheit, tachycardic and hypotensive. The patient was saturating on room air at 99% with no usage of accessory muscles. Initial labs were significant for parasites on blood smear(Image 1), parasitemia of 18%, thrombocytopenia, elevated creatinine, anemia, and elevated lactic dehydrogenase. Plasmodium falciparum was identified. Chest X-ray was done in the emergency department which showed no acute findings. The patient was diagnosed with severe malaria and started on quinine and doxycycline. The patient’s parasitemia was trending down to 1.5 percent several days later, but the patient developed acute respiratory distress with hypoxia. Patient began to desaturate to the mid 80s on room air. Chest X-ray was repeated which showed bilateral lower lobe infiltrates. CT chest was done, which revealed pulmonary edema and bilateral pleural effusions(Image 2). ECHO was also done which showed elevated pulmonary hypertension, with normal EF and no valvular dysfunction.
Discussion: Respiratory distress and lung manifestations have been associated with severe plasmodium falciparum malaria in about 25% of adults (1). Onset of symptoms can begin either prior or after treatment even with improving parasitemia. The mechanism of lung injury involves an increase in the alveolar permeability, which causes fluid loss from intravascular capillaries into the lungs (2). In 2018 the United States had 1,823 cases of confirmed malaria (3). Although a relatively rare diagnosis in the United States, severe malaria can be deadly because of acute lung injury, hence it is important to recognize and begin treatment early to prevent mortality. Although this patient made a full recovery with quinine and doxycycline, intravenous artesunate has shown to reduce the risk of death in patients with severe malaria compared to quinine(4). Intravenous artesunate is the treatment of choice in severe malaria, but is not easily accessible in small community hospitals.
Conclusions: I presented a case of a 32 year old healthy male with severe plasmodium falciparum malaria complicated by acute respiratory distress with findings of pulmonary edema and bilateral pleural effusions on CT scan who was treated at a community hospital with quinine and doxycycline. Severe plasmodium falciparum malaria with pulmonary manifestations has a high mortality rate and it is shown that intravenous artesunate decreases mortality when compared to quinine. Early recognition and easier accessibility to artesunate could be the key to improving outcomes.