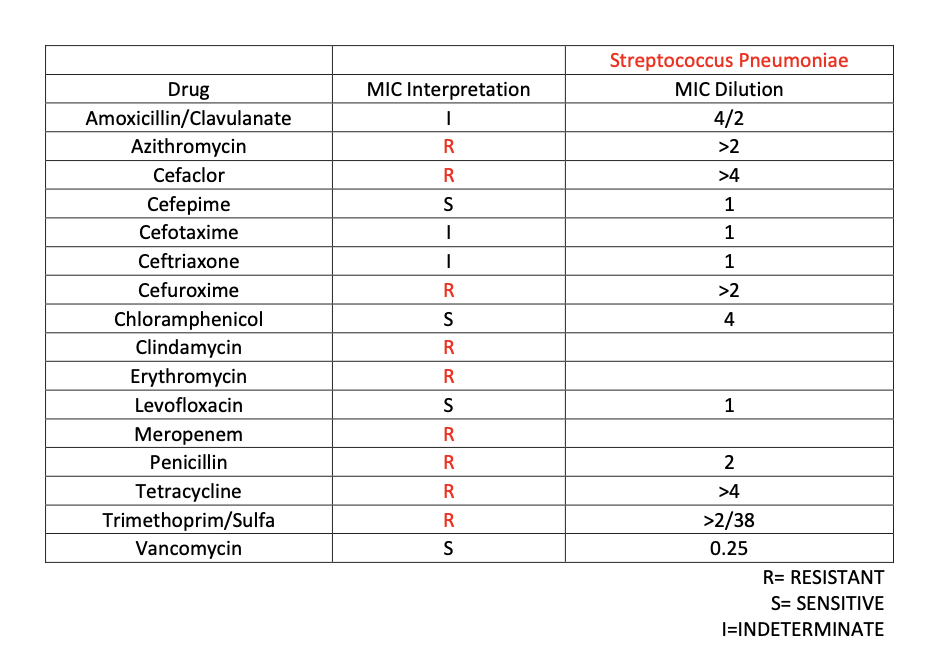
Case Presentation: Patient is a 37-year-old male with a history of HIV, Kaposi’s sarcoma, substance abuse, Hepatitis C, and heart failure. Patient was previously treated for cryptococcal meningitis, neurosyphilis, VZV encephalitis, and ESBL UTI. He presents to the hospital due to shortness of breath, facial pain, malaise, neck stiffness, and abdominal pain with bilious vomiting. Patient states that symptoms have been present for three days. Patient was seen to be in septic shock was transferred to the ICU and started on IV fluid resuscitation and empiric cefepime and vancomycin. At this time, chest X-ray showed evidence of bronchiolitis and airway inflammation. Otherwise, imaging was unremarkable. On admission, WBC count was 26.1, with a neutrophilic predominance, and bandemia. Initial blood cultures grew multidrug-resistant Streptococcus pneumoniae sensitive to vancomycin, cefepime, and levofloxacin. Patient was also seen to have a CD4 helper absolute count of 0. Infectious disease recommended to remove right chest port-a-cath and start the patient on IV Vancomycin and Cefepime. Cardiology was consulted to rule out endocarditis and both transthoracic were negative. Patients’ symptoms slowly improved with supportive care and IV antibiotics and a decision was made to place a PICC line for continued antibiotic therapy.
Discussion: This patient was immunocompromised due to his active HIV infection and complex medical history. The combination of his risk factors all contributed to severe infection. However, an infection with multi-drug resistant streptococcus pneumoniae is highly unusual regardless of risk factors. This case is unique due to the presence of such a significantly resistant organism in the United States and the implication such a disease has on hospital treatment, prevention, and antibiotic utilization. Streptococcus pneumoniae has increased resistance worldwide in the setting of increased antibiotic use. Beta-lactamase, macrolide, fluoroquinolone, and meropenem resistance all pose a significant challenge in treatment. Overall risk factors for multi-drug resistance include but are not limited to chronic disease, repeated exposure to antibiotics, and Immunosuppression (Cillóniz et al., 2018).Clinical implications of resistance are multifold. Resistance is more likely to lead to treatment failure and worse outcomes. Additionally, multidrug resistance has a larger impact in the community as it risks further infection. It is important to prevent multidrug resistance by appropriate usage and preservation of antibiotics. Vaccination with the polysaccharide pneumococcal vaccine is also associated with decreased resistance (Nakano et al., 2018). In this patient, although he had several risk factors, it was important to isolate him and start the appropriate antibiotic regimen. Only with appropriate treatment and identification could the patient and the community be cared for.
Conclusions: This patient’s immunosuppressed state increased his risk of bacteremia through the chemotherapy port specifically in this instance. Multi-drug resistant streptococcus pneumoniae is an extremely rare microorganism regardless of the patient’s predisposing factors, however had traditionally responded to common antibiotic therapy including cephalosporins, macrolides and fluoroquinolones. Due to the high mortality and morbidity associated with those at increased risk, this study aims to bring awareness to the fact that common therapies are exhibiting resistance at a higher rate.