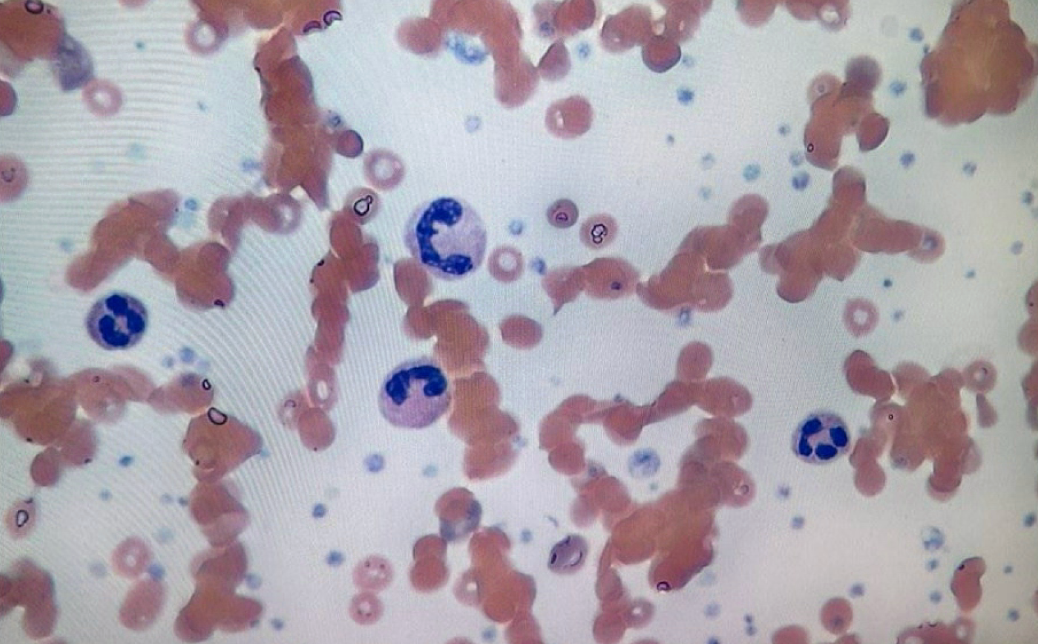
Case Presentation: The patient is a 43-year-old female with asthma, hypertension, and obesity who presented to her PCP for cough, pharyngitis, and dyspnea. Exam revealed jaundice, livedo reticularis, and pallor. Complete blood counts (CBC) showed white blood cells 22.8 x109/ L, hemoglobin 8.9 g/dL, and platelets 674 ×109/L. Her family history had no hematologic malignancies or autoimmune diseases, but remarkable for anemia after chemotherapy in her mother. Patient recently relocated to Massachusetts from Florida,, and now lives in a wooded area with a pet dog. No recent tick bites or sick contacts, but she is a school teacher. Patient denied any acute bleeds and noted her menses to be regular.Patient was sent to the emergency department, where repeat CBC showed worsening leukocytosis to 31.7 8 x109/L and anemia with Hgb of 7.2 g/dL. Consolidation noted on CT chest prompted empiric community acquired pneumonia treatment. Serial mycoplasma IgG was positive and down-trending. First line therapy of warmed red blood cell (RBC) transfusions had limited effect. Significant symptomatic and objective improvement was noted after starting intravenous immunoglobulin (IVIG) 1 g/kg for 2 days and prednisone 1 mg/kg daily for 7 days. She required no further transfusions and was discharged home with outpatient hematology follow-up.
Discussion: Cold agglutinin hemolytic anemia is a rare subtype of autoimmune hemolytic anemia. It can be primary or secondary in nautre. Secondary etiologies include infections, autoimmune diseases, lymphoproliferative disorders, and solid cancers (1). This patient’s hemolysis and agglutination continued after treatment for pneumonia, suggested primary disease. However, consolidation on chest imaging and decreasing M. pneumonia IgG is seen in recent resolving infection per Infectious Disease consultants. This is more consistent with secondary disease, which rendered this case difficult to classify. The most studied drug for CAD is rituximab and is considered first-line (2). Less common treatments include IVIG, corticosteroids, and eculizumab. The use of IVIG for cold agglutinins has been successful in inhibiting hemolysis (3). Corticosteroid therapy is not recommended for primary CAD given the need for long-term high doses to maintain a sufficient response (4). Thus, the treatment plan of this patient included short-term high-dose steroid use in conjunction with IVIG as a bridge to long-term monoclonal antibody therapy. In the DECADE trial, inhibition of terminal complement activation by eculizumab was shown to be well tolerated and led to a significant reduction in hemolysis (5), which may be safer than rituximab (6).Additionally, an increased risk of venothromboembolic events in patients with CAD compared with non-CAD individuals has been reported (7). Folic acid supplementation to prevent folic acid deficiency and ensure ongoing compensatory erythropoiesis has been found to be beneficial in CAD (8).
Conclusions: This case highlights the variable objective data which help differentiate primary vs secondary causes of CAD. The importance of VTE in CAD despite profound anemias are discussed here. Treatment tiers include temperature management, IVIG and limited of steroids for acute severe disease, and Eculizumab and Rituximab for definitive management.