Background: Continuous multiparameter, physiologic monitoring may improve patient outcomes in the medical-surgical wards by identifying patients who need clinical evaluation and or intervention. Alarms may be actionable or non-actionable dependent on whether the alarm is technical in nature or represents a substantive change in patient condition. Alarms will enhance patient care when followed by provider actions which improve the clinical condition of the patient and facilitate continued recovery. Our goal was to identify the number and type of alarms associated with a physiologic alarm system and the associated clinical interventions in surgical units.
Methods: With Cleveland Clinic IRB approval and consent, we enrolled patients in a surgical ward pilot study of a wireless, wearable continuous physiologic monitoring system (PortraitTM Mobile, GE HealthCare, Chicago, IL, FDA 510k cleared August 11, 2023). Prior to patient enrollment, the monitoring system alarm threshold settings were configured with the help of alarm burden analytic software to optimize clinical utility. The monitoring system acquires continuous respiratory rate, pulse rate, and oxygen saturation data. Patients were fitted with the system and randomized to blinded or unblinded monitoring. Those in the blinded group were managed with routine care with bedside vital signs assessment every four hours. Those randomized to unblinded monitoring had continuous vital sign data continuously screened by physician investigators who alerted nurses when vital signs values exceeded study thresholds.
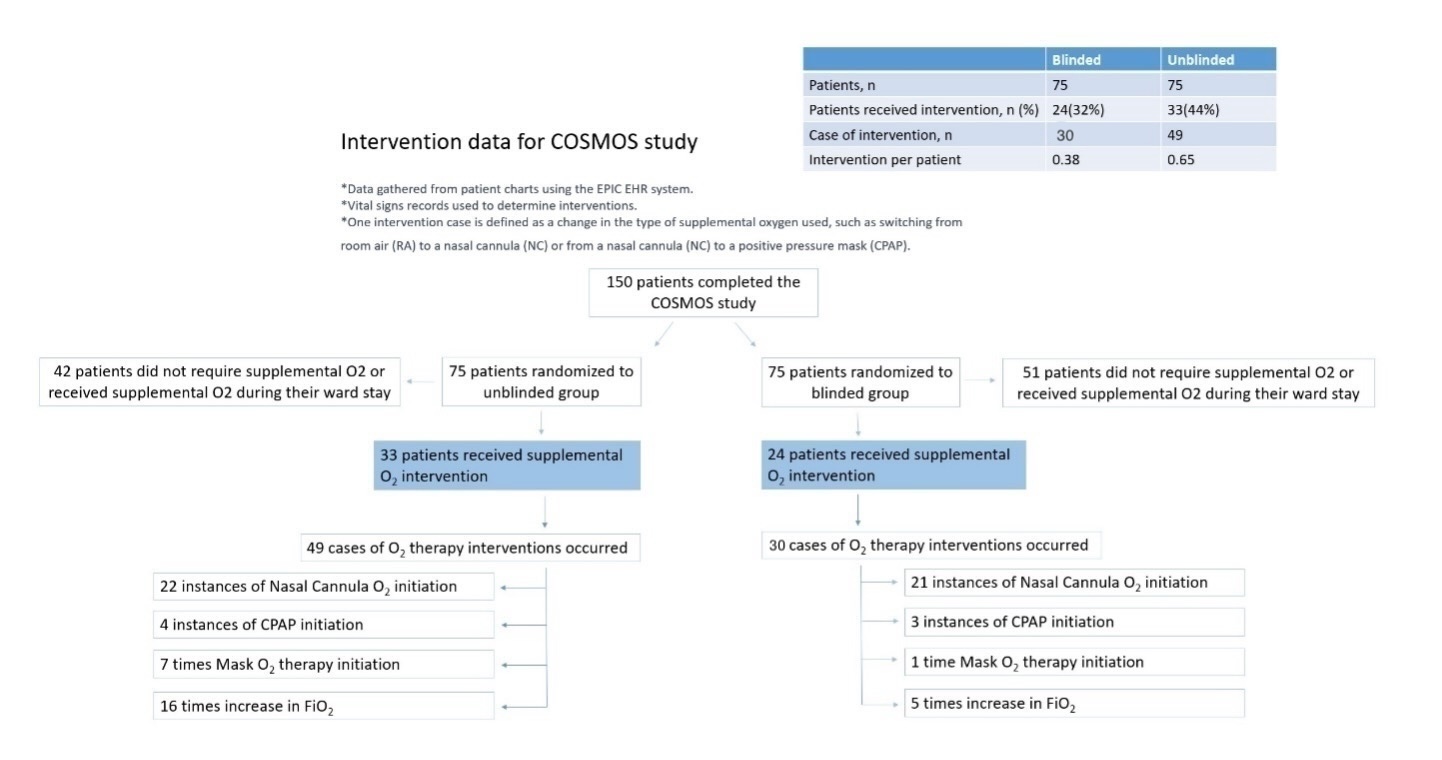
Results: 150 patients were enrolled ,75 each to blinded and unblinded monitoring. In the unblinded group, there were a total of 73 alarms in 33 patients equating to approximately 1 alarm per day per study group patient. Patients with alarms averaged 2.3 alarms per day. 60 unblinded alarms (82%) were categorized as informative, important, or critical by the responsible nurse. 13 alarms (18%) were considered false or distractive. The ratios of interventions to alarm counts were 10/30 for informative alarms, 21/28 for important alarms, and 2/2 for critical alarms. The most common type of intervention was initiation or titration of supplemental oxygen which included nasal cannula, oxygen face mask, FiO2 titration, or CPAP initiation. Blinded and unblinded groups differed in oxygen intervention type and frequency (Figure 1). Supplemental oxygen was applied to 33 (44%) unblinded and 24 (32%) blinded patients. 30 oxygen interventions (0.39/patient) took place in the blinded group versus 49 (0.65/patient) in the unblinded group. Interventions took place in the following blinded/unblinded ratios: nasal cannula initiation 21/22, CPAP initiation 3/4, mask oxygen initiation 1/7, and increase in FiO2 5/16.
Conclusions: Patients with unblinded, continuous physiologic monitoring averaged approximately 1 alarm per day and 82% of alarms were considered informative, important, or critical. The unblinded patients had more oxygen-related interventions. Additional study is required to determine whether increased interventions due to continuous monitoring improves patient outcomes. Further refinement of the monitoring technology and clinical configurations may optimize the number of alarms, clinical workflow, and patient outcomes.