Background: The social determinants of health (SDOH) have been shown to be independent predictors for higher rates of heart failure hospital admissions, lower outpatient follow-up, and poorer health outcomes.1-3 One strategy for addressing the SDOH that has demonstrated promising results in decreasing hospitalization rates and average lengths of stay for patients with chronic illnesses is the involvement of community health workers (CHW), defined as trained community members who provide patients with social support and assist in the navigation and coordination of care.4-7
Methods: A pilot transitional heart failure clinic was opened at an urban academic center with the goal of decreasing hospital readmissions for patients with heart failure by targeting SDOH barriers and improving access to outpatient care utilizing CHWs. A CHW team identified suitable patients for clinic enrollment from the working DRG (drug related group) based on provider documentation and list of high utilizers provided by the insurance companies. Patients were evaluated for the presence of housing, food, utilities, financial, transportation, understanding healthcare, and safety needs through a SDOH screening questionnaire. CHWs developed longitudinal relationships with patients through visits during hospital stays, presence at clinic appointments, and check-in calls to identify and address unmet SDOH needs. All patients were offered transportation to and from clinic appointments, parcels of fresh food, health education, and access to social work services at clinic visits. In order to evaluate the impact of the clinic, 30-day pre/post-enrollment all-cause emergency department visits and readmissions were monitored for each patient. Additionally, clinic show-rates were also tracked.
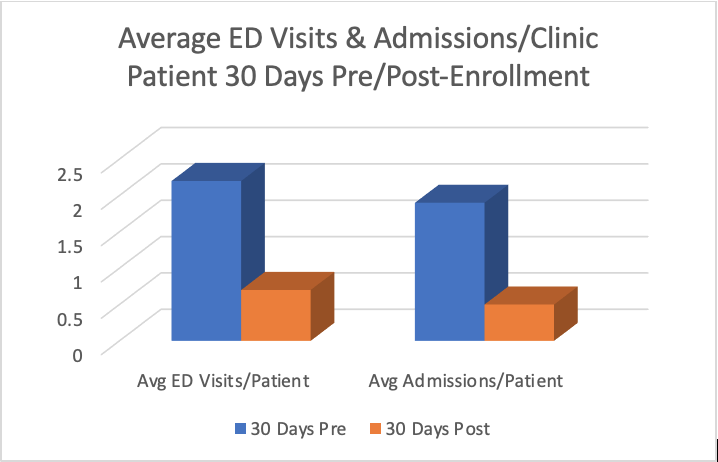
Results: From June 11th, 2020 through September 10th, 2020 33 patients were offered enrollment in the clinic. 23 patients elected to participate and attended at least one appointment. 27 patients completed a SDOH screening questionnaire with the top three needs shown to be: understanding healthcare in 37%, transportation barriers in 14.8%, and food insecurity in 14.8% of patients. After participation in the clinic, the percentage of patients with all-cause emergency department visits 30 days pre/post-enrollment dropped from 95.7% to 43.5%. The average number of emergency department visits per participant decreased from 2.2 to 0.7. Patients with all-cause hospital readmissions 30 days pre/post-enrollment similarly dropped from 95.7% to 39.1%. The average number of hospital readmissions per participant decreased from 1.9 to 0.5. Finally, the clinic show rate was 77.9%, higher than average clinic show rates which are typically in the 50-60% range at our institution.
Conclusions: A substantial portion of patients admitted for heart failure in our institution were found to identify SDOH needs on screening questionnaire with understanding healthcare, transportation, and food insecurity being the top needs. A CHW-driven transitional heart failure clinic that worked to address these SDOH needs through interventions like the provision of transportation, fresh food, patient health education, and social worker access was implemented. Patients enrolled in this clinic exhibited significantly higher than average clinic show rates and decreased 30-day all-cause emergency department visits and hospital readmissions after participation. In the future, we hope to apply this to an expanded patient population to further evaluate the impact.