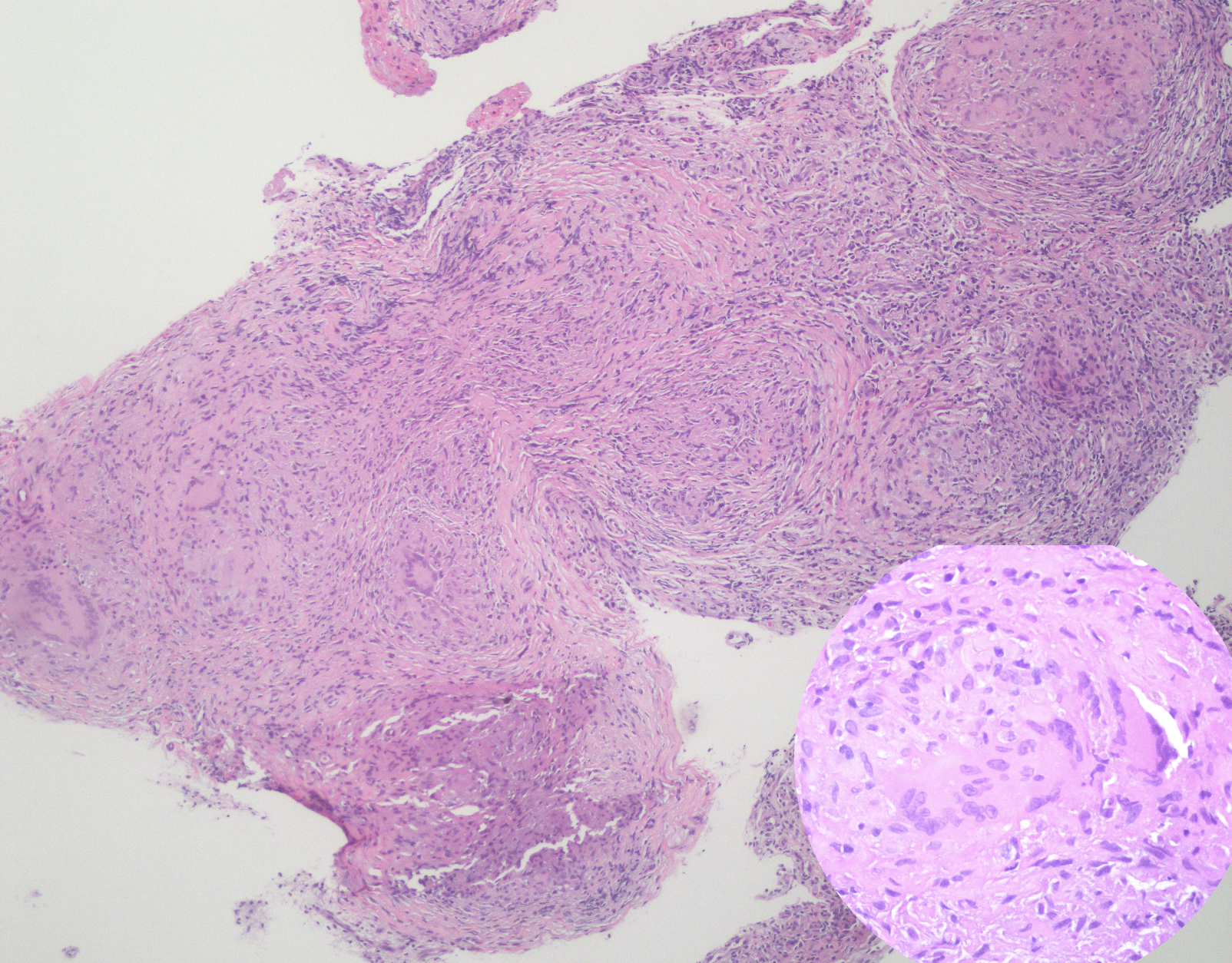
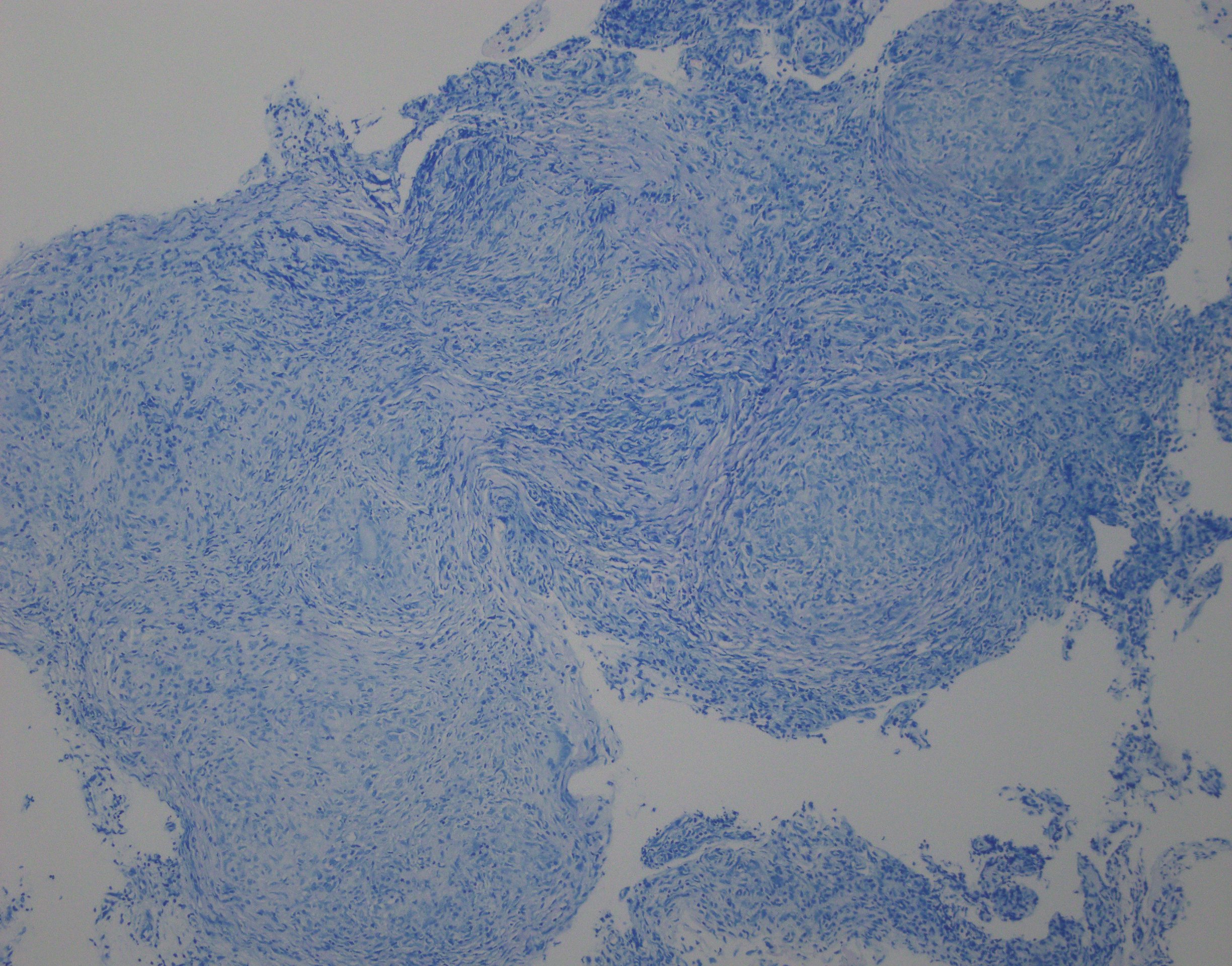
Case Presentation: A 22 year-old female from Guyana with no past medical history presented with shortness of breath, pleuritic chest pain, and dry cough x 5 months. She was treated for community-acquired pneumonia 6 months earlier, though her symptoms persisted. She had an exercise tolerance limited to one block, subjective fevers, malaise, and unintentional weight loss of 15 lbs. On presentation, she was afebrile, normotensive, tachycardic (P 132), tachypneic (RR 25), and hypoxic (SpO2 91% on room air). Exam was notable for BMI 17, increased work of breathing, and decreased breath sounds at the right lung base. Chest X-ray showed a large right-sided pleural effusion and enlarged cardiomediastinal silhouette. EKG showed sinus tachycardia with low voltage. TSH was normal; troponin was negative. Bedside echocardiogram showed a large pericardial effusion with concern for early tamponade, so pericardiocentesis was performed. Her large right pleural effusion was also drained. CT chest showed a right loculated pleural effusion with pleural thickening and extensive thoracic lymphadenopathy including anterior mediastinal, paratracheal, subcarinal, cardiophrenic, and hilar nodes. Pleural fluid was exudative; pericardial fluid was hemorrhagic. There were no malignant cells. Fluid and sputum cultures were negative. Serum LDH was normal, and HIV was negative. Rheumatologic workup was negative, including ANA, RF, dsDNA, proteinase 3 antibody, MPO, and CCP. Quantiferon-TB Gold was positive; however, fluid was negative for AFB by PCR, culture, and smear, and pleural fluid ADA was normal. The patient underwent bronchoscopy: BAL culture, AFB, and cytology were negative, but alveolar tissue biopsy revealed non-caseating granulomas and multinucleated giant cells. AFB and fungal stains were negative. Pathology was consistent with sarcoidosis. She was started on prednisone, colchicine for pericarditis, and rifampin for latent tuberculosis.
Discussion: Tamponade is an unusual initial presentation of sarcoidosis. Clinical cardiac involvement occurs in only 5% of patients with sarcoidosis (1), typically affecting the myocardium and manifesting as ventricular tachycardia, conduction abnormality, or cardiomyopathy. The first case of biopsy-proven pericardial sarcoidosis was in a patient with recurrent pericardial effusion (2). The gold standard of diagnosis is biopsy, which is invasive and lacks sensitivity due to sampling. Retrospective reviews have found that pericardial sarcoid may be more common than previously recognized with non-caseating granulomas found in visceral and parietal pericardium at autopsy (3). A recent review confirmed that when symptomatic pericardial disease was the presenting feature of sarcoidosis, all cases (n=11) were of life-threatening tamponade (4).
Conclusions: There should be heightened clinical awareness for pericardial disease, specifically tamponade, in patients with (or as the presenting feature of) sarcoidosis.