Background: Treating alcohol withdrawal in the inpatient medical setting requires timely identification of the severity of alcohol withdrawal so appropriate treatment can be administered. Delayed or missed diagnosis can lead to increased morbidity and mortality, increased cost and length of stay, and ICU admissions. CIWA-Ar is the most commonly used scale, but it is lengthy and prone to subjectivity. It is a ten item scale where nine measures are ranked from 0 to 9, and one is ranked from 0 to 4. BAWS is a five item scale developed by Darius Rastegar et al. Agitation, sweats, tremor, orientation and hallucinations are graded on a scale of 0 to 3, and hallucinations is one category regardless of type of hallucination. We compared BAWS to CIWA-Ar to see if the scales were similar for predicting alcohol withdrawal severity given that BAWS is easier to administer and less subjective.
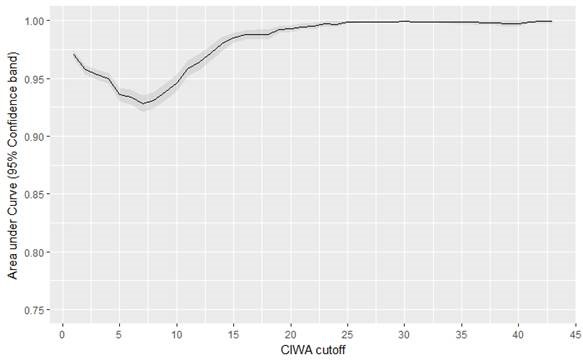
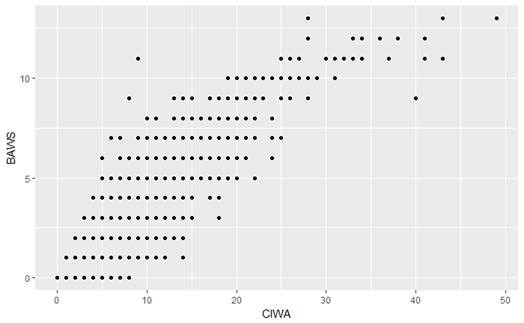
Methods: We created a scale to convert CIWA-Ar scores into BAWS scores and we applied this conversion retrospectively to all CIWA scores obtained in patient encounters on the internal medicine service where a CIWA score was obtained. The data was obtained from EPIC computerized records for all inpatient encounters on the medicine service over a 13 month period with discharge dates between September 1, 2016 and October 25, 2017 (6,478 scores in total). We assessed the ability of BAWS to predict CIWA using area under the curve (AUC) of receiver operating characteristic curves at each CIWA cutoff, along with Cohen’s kappa for CIWA>=12 and >=15.
Results: Using BAWS to predict a range of CIWA, we get a high AUC of 0.92. When we compare a BAWS of 3 to a CIWA of 8 (the threshold for treatment with benzodiazepines) we get sensitivity of 0.9 and specificity of 0.8 [95%CI 0.79,0.81]. When we compared high scores, we found that a CIWA of 12 compared witha BAWS of 6 has a Kappa score of 0.71 [0.67-0.74]. For CIWA of 15 and BAWS of 7, we have a Kappa of 0.76 [0.72-0.8].
Conclusions: BAWS can be converted to CIWA scores retrospectively. We conclude that this suggests the prospective use of BAWS versus CIWA allows for adequate assessment of alcohol withdrawal severity to drive treatment in diverse patient populations in a more expedient and objective manner. We encourage increased awareness of this tool for guiding management of alcohol withdrawal in hospitalized medical patients. Further prospective studies are needed.