Background:
Code Blues, or in-hospital cardiopulmonary arrests, are high intensity, often fatal events occurring frequently within the hospital. National data reviews estimate that survival to discharge following an in-hospital cardiac event is about 24.4%. Further analysis has shown lower survival rates when comparing night shift physicians with day shift physicians (20.7% and 27.5% respectively), but this difference could be mitigated by using a standardized team. Our study sought to evaluate whether two standardized, but uniquely structured, resident-led Code Blue response teams had significantly different event outcomes immediately after the event and at discharge.
Methods:
The study was completed at an 800-bed urban tertiary referral academic hospital, where all Code Blue events were responded to and led by a team of Internal Medicine residents. Two different teams of residents ran the events. The “Day Team” is comprised of 5 upper level residents who lead events from 8:00am to 8:00pm Sunday to Thursday and for 24 hours periods on Friday and Saturday. The “Night Team” is a group of 3 interns and 6 upper level residents who work in the hospital only at night from 8:00pm to 8:00am on Sunday until Thursday. All Code Blue events for admitted patients within the hospital from July 2014 until June 2015 that required advanced cardiac life support or intubation were included in the analysis. Events in the intensive care unit, outpatient locations, surgical floors and the emergency department were excluded. The primary outcome evaluated was Code Blue event survival. Secondary outcomes included survival until discharge and discharge disposition. Basic demographic information was also obtained for all of the patients included.
Results:
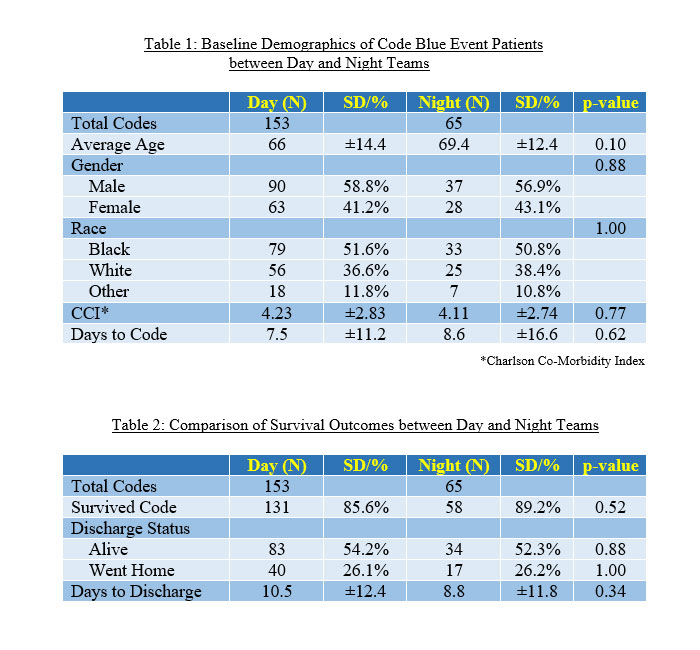
A total of 218 Code Blue events occurred during the study period, 153 (70.2%) by the Day Team and 65 (29.8%) by the Night Team. Average age, gender, and ethnicity were not significantly different between the two groups. The average Charleston Comorbidity Index for the Day team was 4.23 ±2.83 and the Night Team was 4.11 ±2.74 (p=0.77). Code Blue event survival was 85.6% for Day Team versus 89.2% (p=0.52). Day Team and Night team had no significant difference in survival to discharge (54.2% vs. 52.3%, p=0.88) and discharge to home (26.1% vs. 26.2%, p=1.00).
Conclusions:
At our institution, there was no significant difference in Code Blue events in outcomes between a team of residents working primarily in the day compared to those working exclusively at night. The lack of difference may relate to the same pool of senior residents being Code Blue team leaders on both teams throughout the study period, as well as local institution policies in code team dynamics, training and set-up. Overall Code Blue survival rates during the study period were higher than those published in the literature.