Background: The healthcare system needs tools that can predict which patients are at risk of deterioration, before adverse outcomes such as cardiac arrest or even death occur. Many of these patients will show signs of significant physiological deterioration in the 24 hours prior to ICU transfer or cardiac arrest [1-4]. Different scores have been developed to predict these adverse outcomes [6,7], two of them being eCART and MEWS which will be compared in this study.
Methods: The study was conducted in Saint Francis Hospital of Evanston, Illinois. Data was collected from November 22nd 2018 to August 17th 2019 and all rapid responses during this time period were reviewed. We excluded patients that had rapid response (RRT) called but had a code status of DNR/DNI. The primary outcome was set as cardiac arrest, ICU transfer or death within 24 hours of activation of RRT. Patients were divided into two categories: ones that had adverse outcome after RRT versus ones that didn’t have an adverse outcome and remained on the general medical floor after 24 hours of RRT activation.Two early warning scores were compared in this study, MEWS and eCART, and comparison was done with calculation of accuracy of each of these scores in predicting adverse outcome (cardiac arrest, ICU transfer or death within 24 hours). Statistical analysis was done using PSPP software (GNU PSPP Statistical Analysis Software Release 1.2.0). MEWS more than 4 and 5 [5] versus eCART more than 94 or 97 (as established in our institution) were set as intermediate and high risk groups respectively.
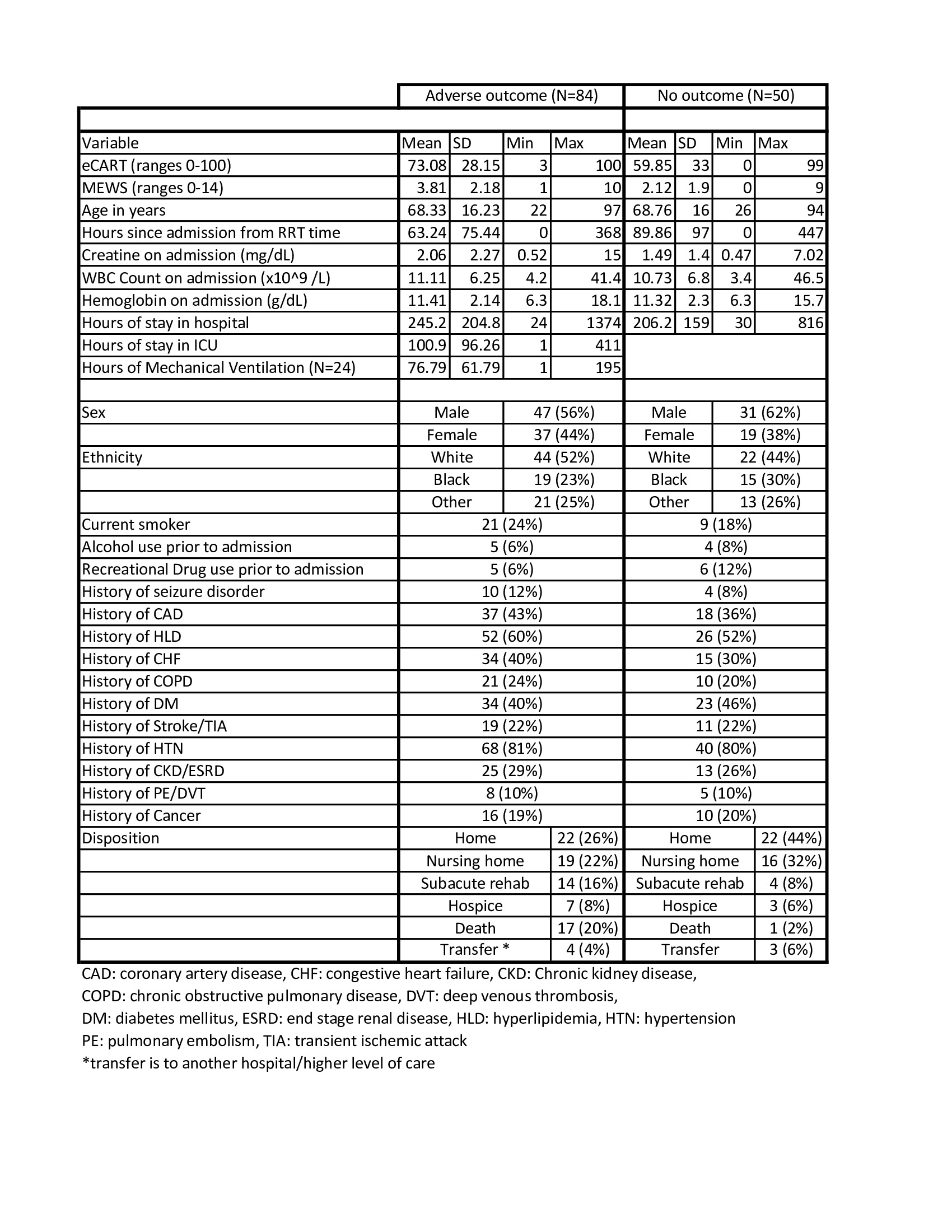
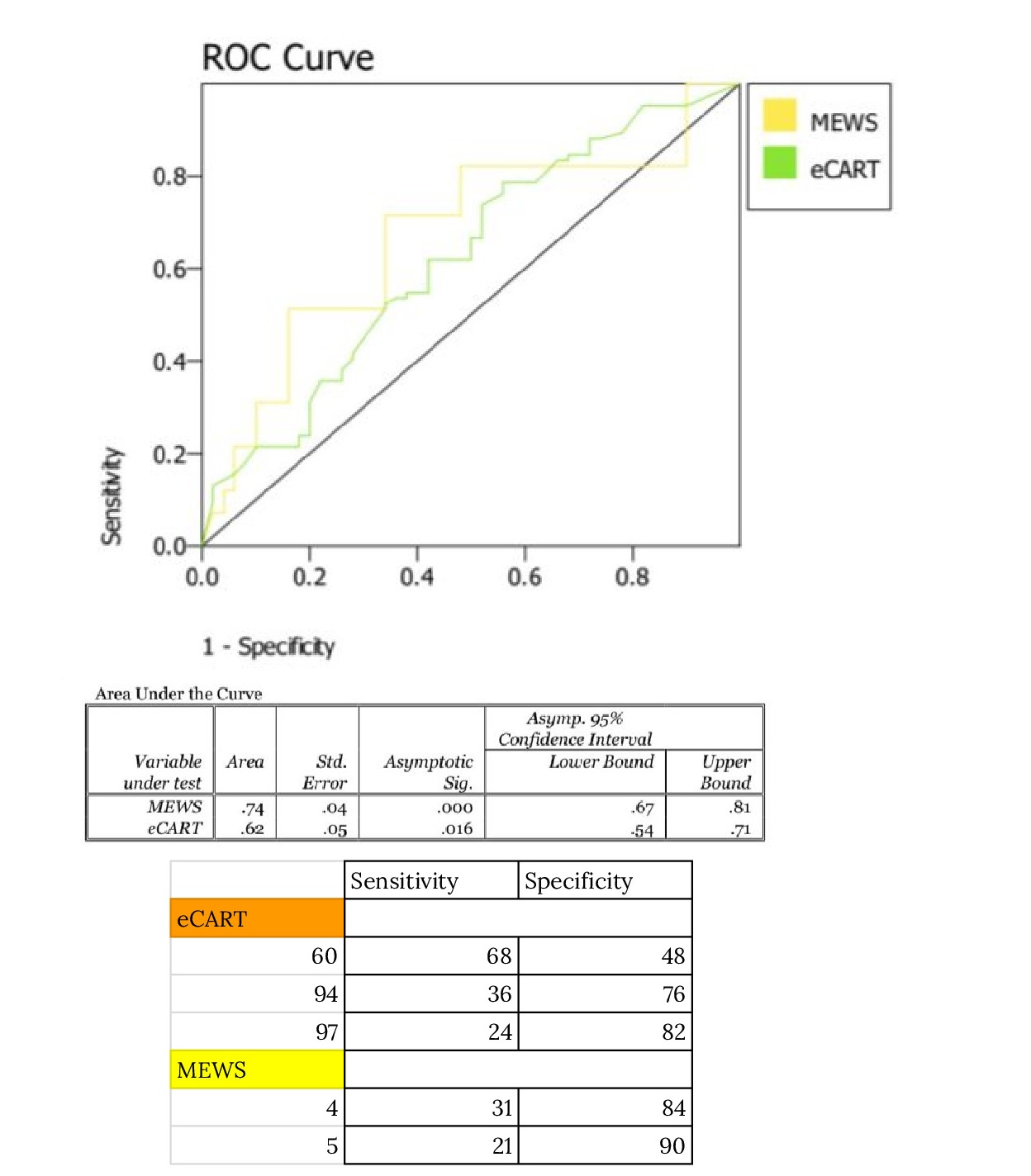
Results: 144 patients that had RRT called from January 22nd 2019 to August 17th 2019 were included. 10 were excluded due to DNR/DNI status. 84 patients had an adverse outcome within 24 hours after RRT. Mean hospital stay was 245.23 hours for the adverse outcome group versus 206.18 hours for the group that had no adverse outcome. More patients were discharged to home in the latter group.AUC for eCART was 0.62 (95% CI 0.540 – 0.710) and AUC for MEWS was 0.74 (95% CI 0.670 – 0.810). Specificity for an eCART value of 60, which was considered high risk in the study conducted by Churpek et al [7], was 48%. In their study they found a specificity of 95% which is a significant difference from our study. Specificity was 76% for an eCART value of 94 versus 84% for a MEWS score of 4. Specificity was 82% for an eCART value of 97 versus 90% for a MEWS score of 5. Sensitivity was 36% for an eCART value of 94 and 24% for a value of 97. It was 31% for a MEWS score of 4 and 21% for a score of 5. eCART value of 60 had a sensitivity of 68%. There was a significant decrease in the number of RRTs after eCART was available. There were 90 RRTs called from January 22nd 2019 to July 31st 2019 (post eCART era) and 158 RRTs called from January 22nd 2018 to July 31st 2018 (pre eCART era).
Conclusions: MEWS score calculated at the time of RRT had higher accuracy in predicting adverse outcomes within 24 hours of RRT activation than eCART score. Due to the contradiction in findings as compared to prior studies [7,8,9] more research is needed to compare these two scores.Fewer RRTs occured since the implementation of eCART in our hospital and this is likely because we have real time access to patients’ eCART scores, even before RRT or adverse outcomes occur. This could lead to more interventions being done prior to a patient’s deterioration when eCART values are generally high for a patient and could in fact mean that eCART is better than MEWS score in preventing rather than predicting adverse outcomes.