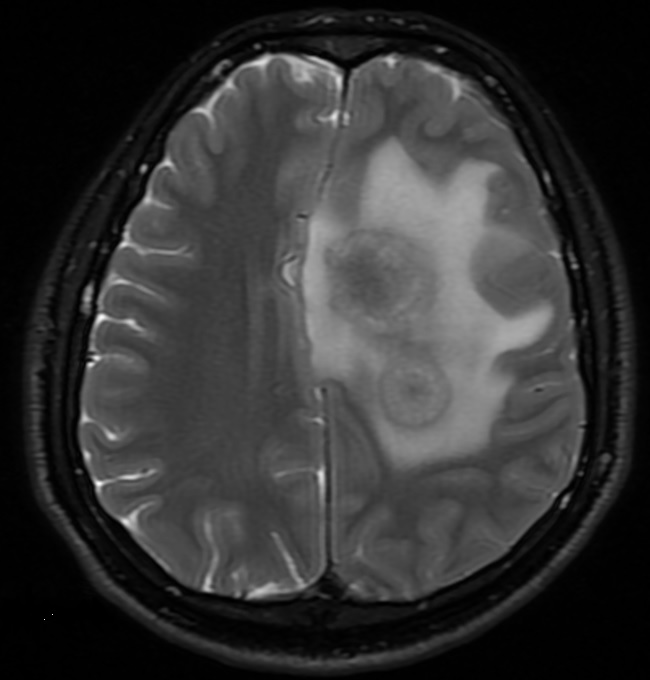
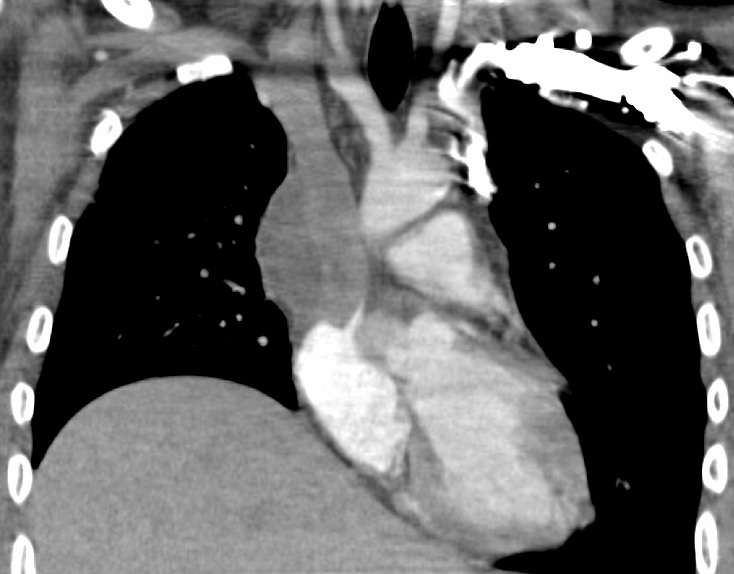
Case Presentation: A 25-year-old previously healthy male presented with two weeks of right arm and leg weakness, paresthesia, difficulty walking, and low-grade fever. Head CT revealed two masses in the superior left cerebral hemisphere. Head MRI showed two intensely enhancing masses measuring 2.6 x 2.7 cm and 1.6 x 1.7 cm with marked surrounding edema and a 0.6 cm midline shift. Initial management was IV dexamethasone and levetiracetam. Labs revealed a white blood cell count (WBC) of 12,600 with a 1+ left shift. An intracranial stereotactic biopsy was performed, which demonstrated scanty leukocytes. He subsequently underwent an image guided left frontal craniotomy with intraparenchymal mass resection. Flow cytometry showed a predominance of T-cells with a moderate amount of plasma cells and numerous sepatate fungal hyphae amongst granulomatous inflammation and fibrosis. Analysis revealed the mass to be composed of Aspergillus flavus and Propionibacterium acnes. He was managed on voriconazole, micafungin, ceftriaxone, and dexamethasone. HIV 1 and 2 antibodies and p24 antigen were non-reactive. The micafungin was later discontinued given the lack of evidence of dual therapy in a immunocompetent patient with invasive cerebral aspergillosis. The P. acnes culture was later felt to be a potential contaminant, but a full duration of antibiotics were provided because there are case reports of this organism causing brain abscesses. During the hospitalization he began experiencing new onset bilateral arm edema with rigidity and neck fullness. There was a concern for superior vena cava (SVC) syndrome. Chest CT revealed SVC/mediastinum mass measuring 5.2 x 3.9 x 3.7 cm. Cardiothoracic surgery debulked the mass, removed the superior vena cava, and used a homograft to connect the innominate vein directly to the right atrium. Pathology report showed abundant hyphal organisms with necrotizing granulomatous inflammation. Post-surgical course was complicated by diffuse ST segment changes, confirmed with 12 lead ECG, and elevated troponin, thought to be secondary to the surgery. Patient was asymptomatic. ST segment and troponin levels normalized without further intervention. He was discharged clinically stable on voriconazole.
Discussion: Disseminated Aspergillosis is rare in immunocompetent adults. It has a predilection for the lungs, often seen in immunocompromised patients in the presence of preexisting lung disease, recipients of solid organ or stem cell transplants, hematologic malignancy, chronic high dose steroids, or neutropenia. To the best of our knowledge this is the first case of an immunocompetent patient presenting with both cerebral aspergillosis and SVC syndrome secondary to invasive Aspergillus flavus. Studies indicate invasive aspergillosis is rising and has a poor prognosis despite antifungal therapy. This patient had a favorable outcome with neurosurgery and cardiothoracic surgical intervention concurrently with voriconazole.
Conclusions: Hospitalist frequently provide care for patients with brain and/or chest masses. Infectious causes, including rare manifestations, should be on the differential diagnosis. As our case indicated, invasive disseminated aspergillosis can occur in immunocompetent patients. Prompt surgical intervention when indicated and appropriate antifungals are lifesaving.