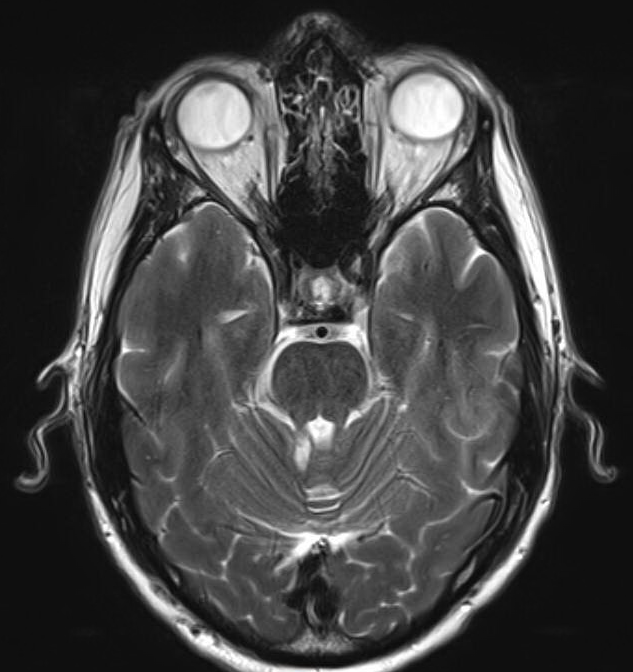
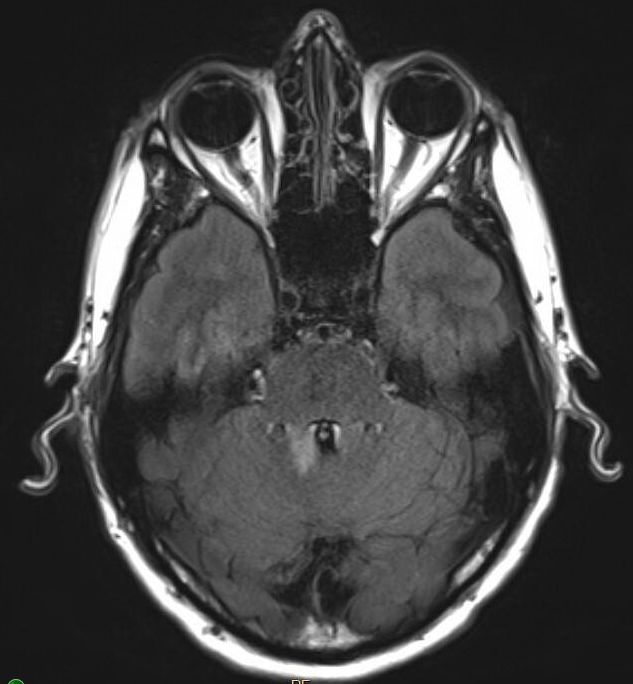
Case Presentation: We report a case of subacute progressive cerebellar ataxia in a 56-year-old male with significant smoking history and COPD, presenting 3 weeks after the start of dizziness and gait ataxia. The patient had associated dysmetria and balance issues, which progressively worsened prompting admission to an outside hospital. There, a CT head was found to be unremarkable, however a CT chest with contrast was significant for incidental bilateral pulmonary embolism, but negative for mass. MRI of the brain was concerning for multiple deep and subcortical white matter hyperintensities on FLAIR sequence, most prominent in the R cerebellum and into the R pons. Due to concerns for a demyelinating process, the patient was transferred to our hospital for a higher level of care. Serum studies for autoimmune criteria were immediately drawn and demonstrated elevated titers for Rheumatoid Factor (nonspecific for autoimmune etiology) and anti-TPO antibody (though a normal anti-Thyroglobulin made Hashimoto’s encephalopathy less likely). Due to concerns for malignancy, a CT abdomen and pelvis with contrast as well as US scrotum were pursued which were negative for masses. A lumbar puncture was performed which showed elevated oligoclonal bands, but was minimal and non-diagnostic of multiple sclerosis. On day 2 of admission he had acute worsening of dysarthria and tremor, and it was deemed necessary to start empiric high dose steroids with plans for plasma exchange for presumed autoimmune cause. Fortunately, he improved significantly on steroids without need for further therapy. He was discharged on a steroid taper. He did have one relapse of symptoms which required another high dose burst with improvement. MRI Cervical and Thoracic spine was performed which was negative for other CNS abnormalities. He continues to be on low dose steroids with further outpatient work-up.
Discussion: Autoimmune cerebellar ataxia comprises a large subset of etiologies for subacute and chronic causes of ataxia. Recognition of this is key to early intervention due to often rapid improvement with immunosuppression. It is often difficult to differentiate etiology of autoimmune cerebellar ataxia due to the wide range of autoimmune causes alone. As paraneoplastic etiologies of ataxia are also responsive to steroids, those with higher risk for malignancy can be screened prior to start of empiric steroids so as not to alter cancer diagnosis or treatment plans due to steroid pre-treatment.. Early imaging, testing, and rule-out of other acute ataxia syndromes such as acute ischemia, hemorrhage, toxin, or infection are crucial to safe immunosuppressive treatment. Once determined safe, treatment with immunosuppression can drastically improve symptoms and decrease chronicity and relapse.. Relapse of autoimmune disease after initial steroid burst can occur, and steroid tapers and adjunct immunosuppression can be beneficial.. Continued outpatient follow-up, repeat imaging, and testing is crucial for definitive diagnosis.
Conclusions: This case demonstrates the variability of autoimmune cerebellar disorders, and the importance of prompt recognition and work-up. Rapid initiation of immunosuppression is crucial for patient treatment and outcome. Definitive diagnosis is difficult and requires extended follow-up.