Background: Academic Medical Centers (AMC) have utilized teams comprised of an attending, resident, interns and medical students to care for hospitalized patients. ACGME work restrictions have reduced the capacity of teaching services. Consequently, most AMCs now rely on direct care Hospital Medicine Services (HMS). Non-clinical tasks (making appointments, faxing for records), traditionally performed by teaching teams, negatively impact the productivity of individual attending driven HMSs. AMCs have approached these inefficiencies in various manners. Since they address non-clinical tasks, there is no suggestion that any model results in better clinical outcomes. Accordingly, we sought to determine which is most cost -efficient.
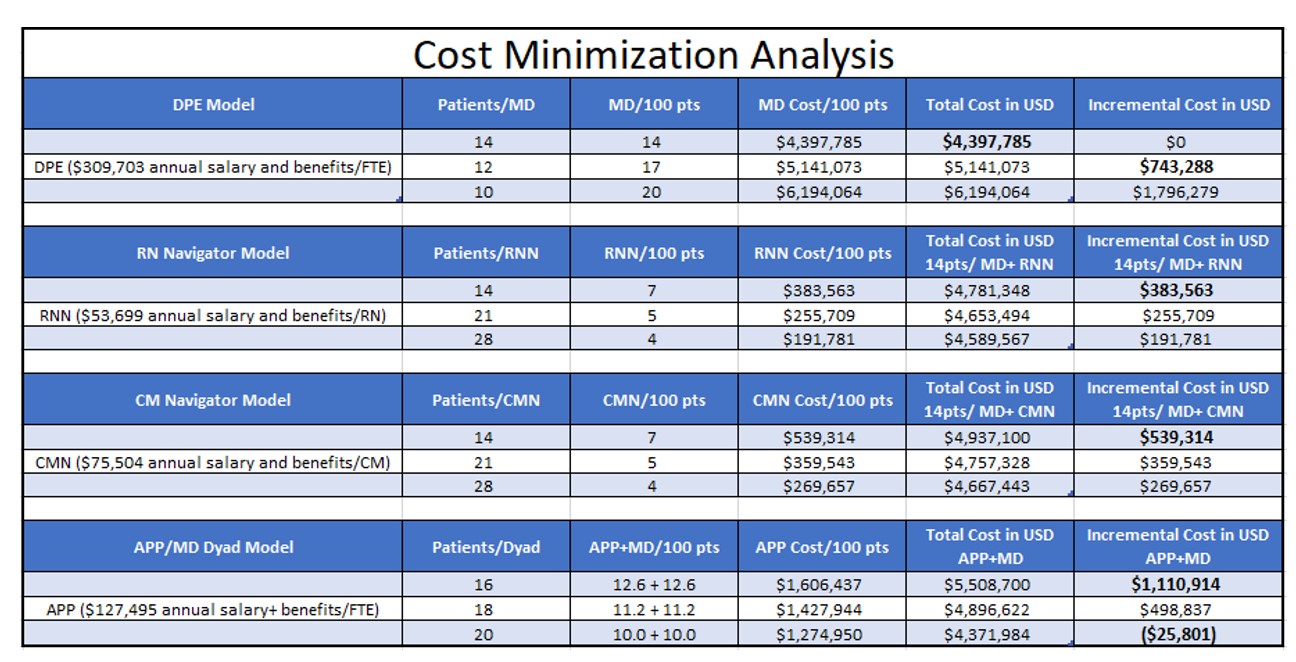
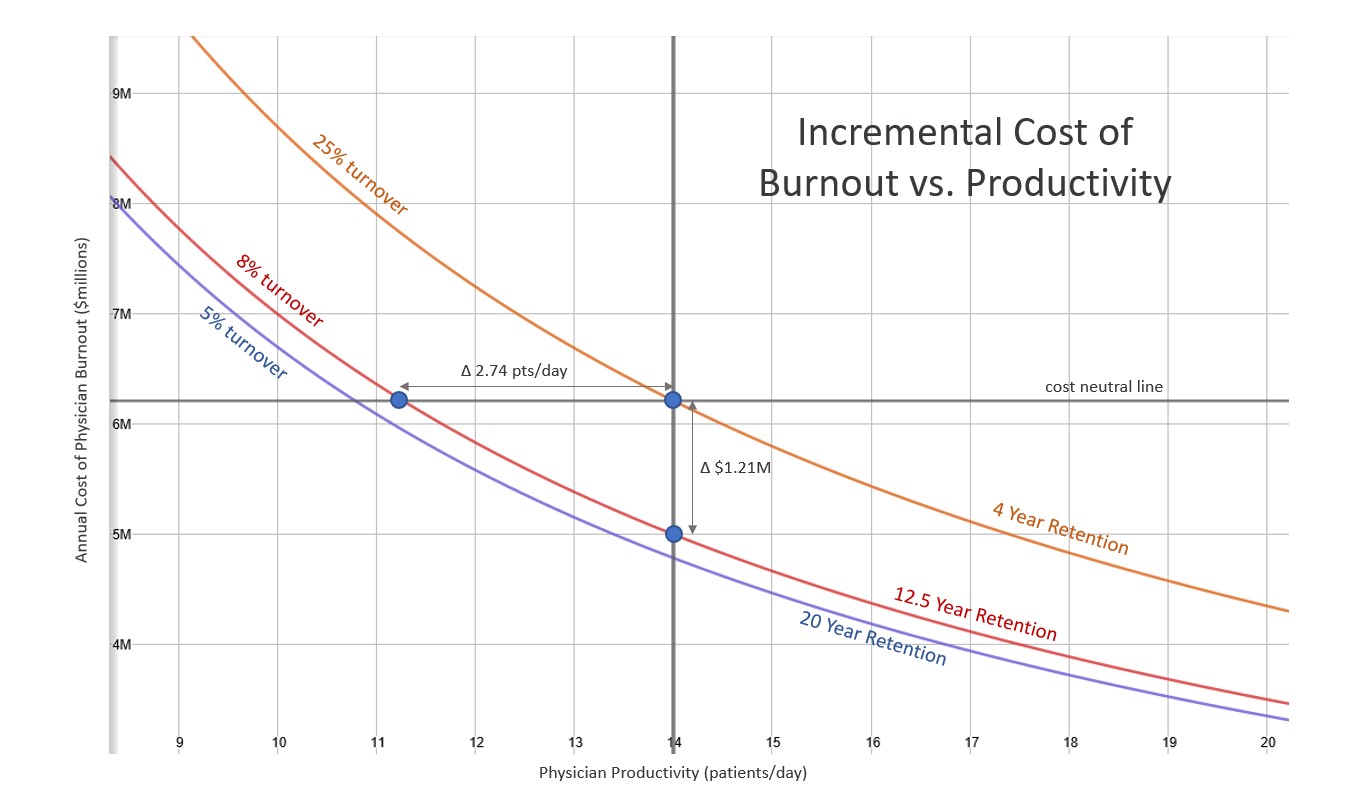
Methods: We performed a cost minimization analysis from the hospital perspective of 4 HMS models – decreased productivity expectations (DPE), nurse or case manager navigators (RNN, CMN), APPs (APP) and tolerating higher turnover (burnout model – BOM). We used 2016 MGMA data to determine compensation and productivity standards. Compensation data for RNs and CMs were obtained on www.glassdoor.com. We included a 20% benefit rate for all providers (Frenz et al). All models were compared to a standard productivity model (SPM) of one hospitalist seeing 14 patients per day and annual costs were determined on the staffing needs to round on a daily census of 100 patients. DPE models one hospitalist caring for 12 patients daily. RNN and CMN models each navigator seeing 14 patients daily. The APP models each APP-MD dyad seeing 16 patients daily. The BOM compared a standard turnover of 8% (12.5-year longevity) to 25% turnover (4-year longevity- Vuong et al). We calculated the incremental costs of the different models as compared to the SPM. Sensitivity analyses were performed to account for reasonable variations in all models.
Results: The annual cost to staff the SPM for 100 patients was calculated to be $4.40 million(M). Incremental, annual staffing costs ranged from $0.38M for the RNN model to $1.11M for the APP model (Table) and $1.21M for the BOM (Figure). The breakeven point for the APP model was 20 patients per dyad daily. DPE to 12 and 10 patients resulted in incremental, daytime annual staffing costs per 100 patients of $0.74M and $1.80M, respectively.
Conclusions: The RNN model is the most cost-efficient approach to staffing direct care HMS in AMCs. Costs in these models can be extrapolated to larger (or smaller) census sizes. Simply reducing productivity expectations is cost-inefficient. Burnout is the most detrimental model.