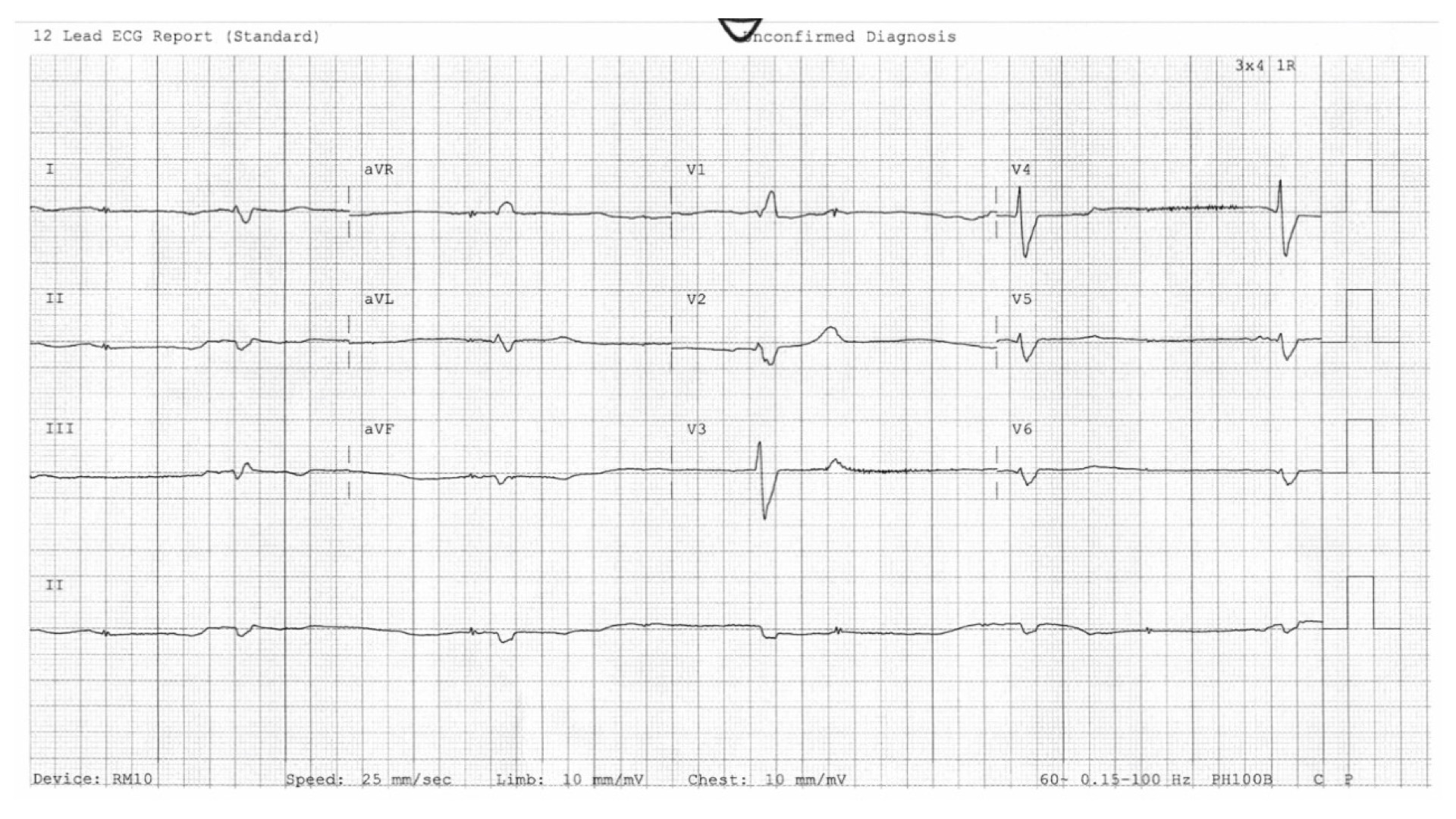
Case Presentation: A 78-year-old man with atrial fibrillation on amiodarone and rivaroxaban, heart failure with reduced ejection fraction (HFrEF) on metoprolol and furosemide, hypertension on amlodipine and lisinopril, type 2 diabetes on metformin, and chronic kidney disease, presented with several weeks of progressive lethargy and confusion in the setting of chronic functional and cognitive decline.He was bradycardic (HR: 30-40), hypotensive (BP: 60-80 over 30-50), and had evidence of significant volume overload. Labs were notable for elevated lactate (7.2), potassium (6.6), serum creatinine (4.1, up from baseline 2.5), and NT-proBNP (>30,000). ECG demonstrated bradycardia with a wide QRS complex. Chest X-ray showed evidence of pulmonary edema. Given marked bradycardia, renal failure, shock, and hyperkalemia in the setting of metoprolol use, he was diagnosed with BRASH syndrome (Bradycardia, Renal failure, AV nodal blockade, Shock, and Hyperkalemia), most likely triggered by HFrEF exacerbation.He remained unstable despite IV atropine, so he was started on an epinephrine drip that improved his hemodynamics. He was given IV calcium, bicarbonate, and insulin for hyperkalemia. Due to his oliguric acute-on-chronic kidney injury, he was transferred to the ICU for urgent hemodialysis to treat his clinically significant hyperkalemia.His lab values normalized, and he was transferred to Hospital Medicine. All of his home medications were held due to concern that these contributed to his presentation. As urine output improved, he was started on IV furosemide for volume overload. Home medications were gradually reintroduced with the exception of amiodarone due to concern for recurrent bradycardia and metformin due to worsened renal function. On discharge, he was euvolemic without recurrence of bradycardia, hyperkalemia, AV nodal blockade, or hypotension.
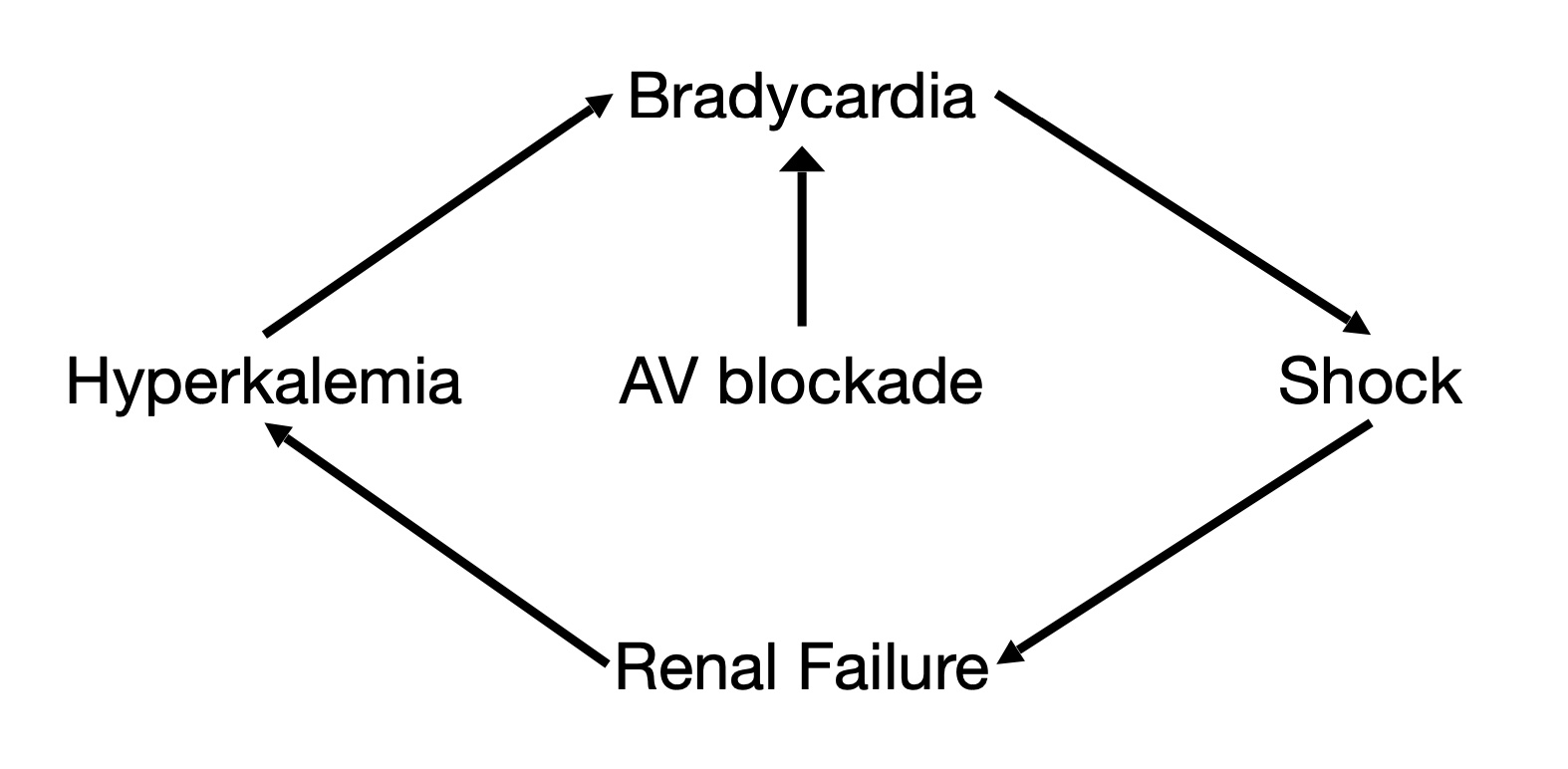
Discussion: BRASH syndrome is defined by Bradycardia, Renal failure, AV nodal blockade, Shock, and Hyperkalemia (1). It is triggered by a synergistic effect of AV nodal blockade and hyperkalemia, which leads to bradycardia out of proportion to underlying nodal blockade, medication effect, or hyperkalemia alone. This severe reduction in heart rate results in poor renal perfusion that further inhibits potassium excretion, exacerbating both hyperkalemia and bradycardia (2).Acute management must simultaneously address bradycardia and hyperkalemia (3). If IV atropine fails to resolve bradycardia, epinephrine is recommended to increase heart rate and shift potassium intracellularly. IV calcium, insulin with dextrose, and bicarbonate are also used to temporize hyperkalemia. Volume status must be assessed to determine whether to pursue diuresis or dialysis for definitive treatment of hyperkalemia. Further management steps should target treatment and prevention of the underlying trigger for BRASH syndrome in each patient.
Conclusions: BRASH syndrome is triggered by the synergistic effect of AV nodal blockade and hyperkalemia. Any patient on AV nodal blockers may present with BRASH syndrome if hyperkalemia or renal failure develops, such that patients with cardiovascular disease on AV nodal blockers and renal disease are at particularly high risk, with relatively subtle and common clinical triggers precipitating this vicious cycle. BRASH syndrome is an important entity to recognize quickly for appropriate intervention to break the underlying pathophysiologic positive-feedback loop that, if uninterrupted, can lead to multi-organ failure.