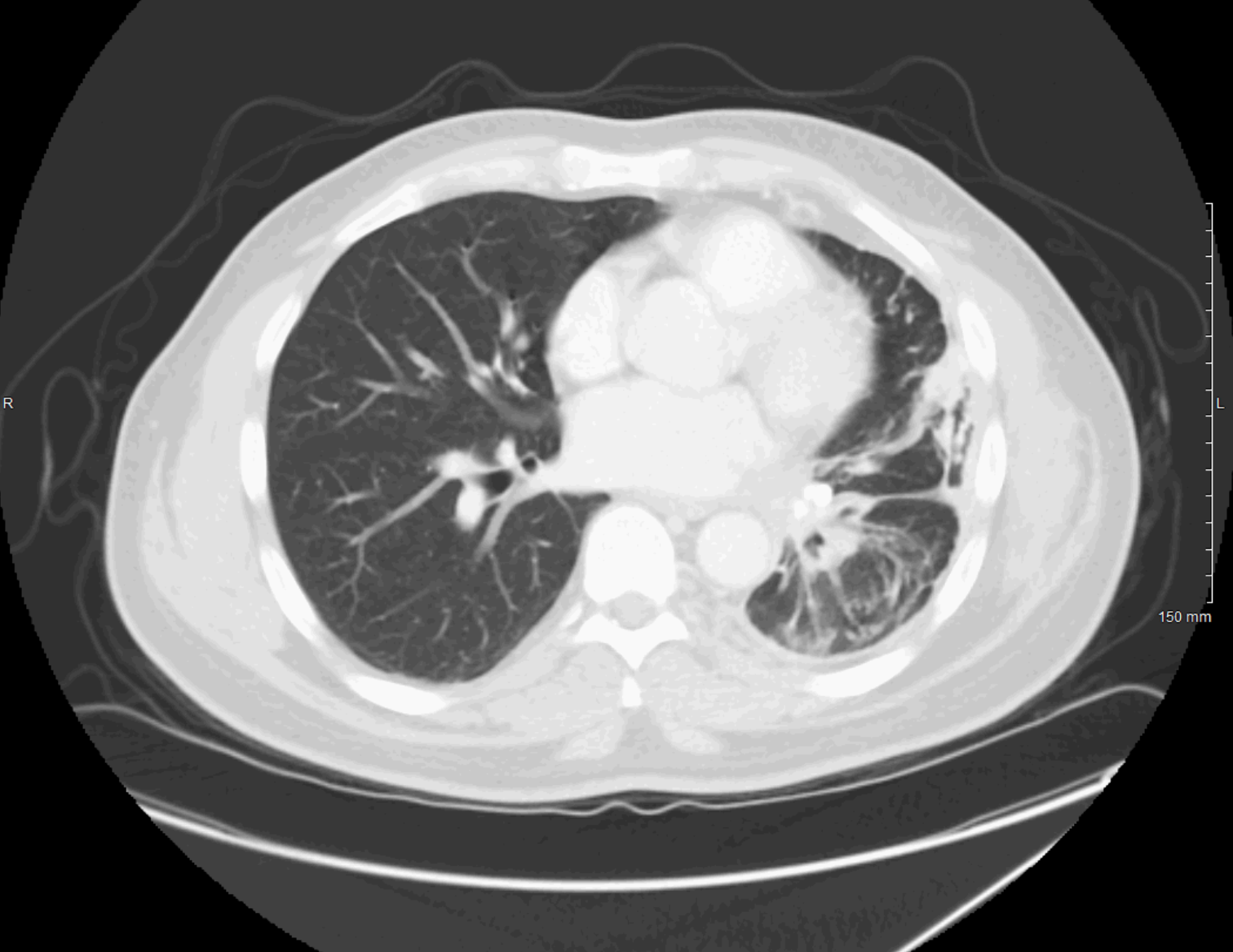
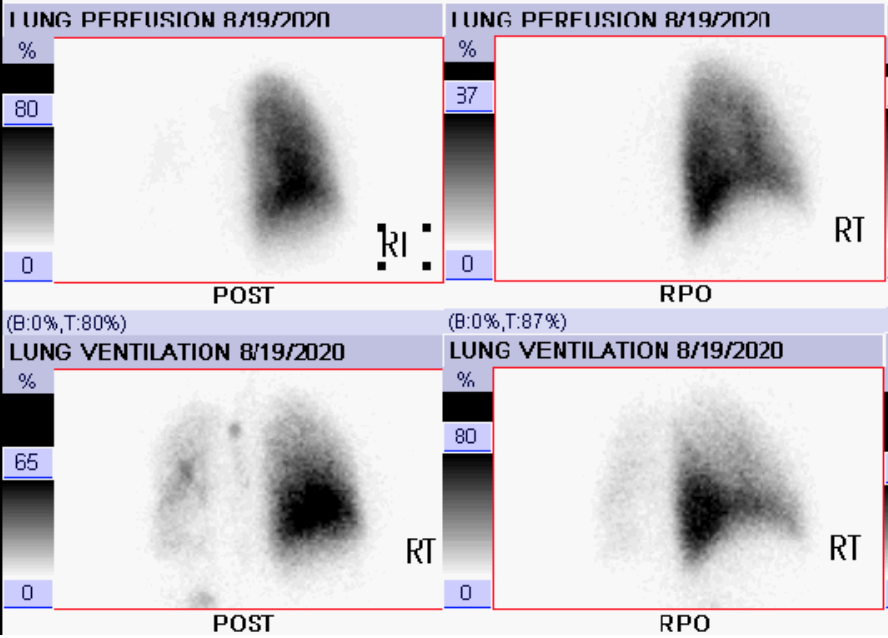
Case Presentation: A 50-year-old African-American male with a past medical history of essential hypertension presented to the emergency department with a 3-day history of worsening substernal chest pain and shortness of breath. He had no fever, chills, cough, recent immobility, or changes in his medications. He was compliant with hydrochlorothiazide. A review of systems was otherwise negative. Vital signs were within normal limits. Physical examination revealed decreased breath sounds throughout the left lung field. Investigations included a CT chest with contrast that revealed pleural thickening in the left hemithorax with narrowing of the left central bronchi and complete occlusion of the left superior and inferior pulmonary veins with extensive collateral formation evident surrounding the central airway on the left. FDG-PET/CT scan revealed hypermetabolic activity in the left hilum. The pulmonology team was consulted and performed a EBUS-TBNA which revealed no malignancy, but revealed extensive fibrosis with chronic inflammation and extensive dystrophic calcifications. Flow cytometry of biopsy was negative. Patient underwent a V/Q scan which revealed no perfusion to the left lung with minimal ventilation (95% perfusion of the right lung and only 5% in the left lung) consistent with essentially absent perfusion of the left lung. Investigations were negative for tuberculosis, histoplasma, and autoimmune causes. Our patient was diagnosed with FM and was started on prednisone 40mg per day with pneumocystis jirovecii prophylaxis (TMP-SMX). Pulmonology deferred placing an airway or vascular stent and he was discharged with outpatient follow-up for both pulmonology and rheumatology.
Discussion: Fibrosing mediastinitis is a life-threatening fibroinflammatory disease characterized by dense fibrotic infiltration involving the mediastinal and hilar regions that can cause narrowing or occlusion of the vital airway and vascular structures within the thorax. The two predominant subtypes are post-histoplasma infection and idiopathic. Geographic distribution is a significant risk factor, especially for those in the Ohio River Valley because of endemic Histoplasma capsulatum. There is great variability in clinical presentation including dyspnea, pleuritic chest pain, hemoptysis, fatigue, dysphagia, or swelling of arms and face. Diagnostic work-up is of vital importance to exclude fibrosing mediastinitis mimics which include active histoplasmosis infection, autoimmune causes [IgG4-related disease], Hodgkin’s lymphoma, mediastinal granulomatous infections, or sarcoidosis. There is no current gold standard therapy for fibrosing mediastinitis. Fibrosing mediastinitis is ideally managed by an interprofessional team that includes a pulmonologist, pathologist, laboratory specialist, and an infectious disease expert, as current management is primarily focused on relieving vascular obstructions and airway obstructions with case-by-case use of corticosteroids and antifungal therapies.
Conclusions: Improving provider knowledge of fibrosing mediastinitis is important because of the atypical presentation and physician unawareness. Although rare, it should be considered in the differential diagnosis of a fibrotic infiltration in the mediastinal or hilar regions. This disease is ideally managed by an interprofessional team who can decide whether a decompressive surgery is needed and can consider the use of corticosteroids and antifungal therapy.