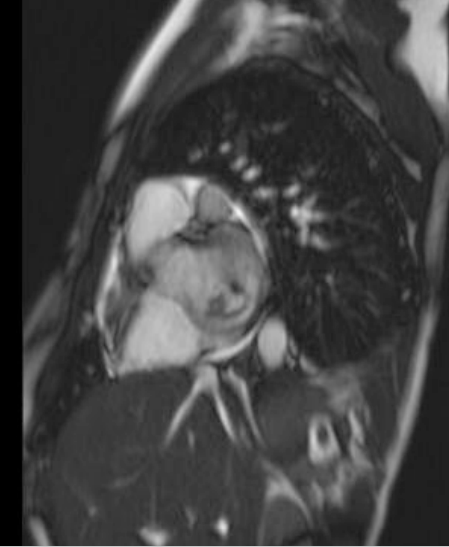
Case Presentation: A 17 year old male recently diagnosed with high risk B-Precursor ALL and induction failure, was found in clinic to have an acute murmur. Three days prior, he had arm and leg aches, dry cough, a single fever and fatigue that improved with blood transfusion. Now he had a 3/6 holosystolic blowing murmur at his cardiac apex. TTE a month ago was normal. His ANC was 332. He received his chemotherapy and was admitted. TTE now showed moderate mitral regurgitation, low normal ejection fraction and a 12mm vegetative mass on the anterior mitral leaflet.
The working differential included thrombus, infectious vegetation or leukemic infiltrate. He had no infectious symptoms and the mass lacked typical vegetation features, so endocarditis was low on the differential. The location of the mass, normal LV function and lack of arrhythmias made clot less likely. Given his failed induction, the mass was thought to be leukemic infiltrate. Blood cultures were negative, and he had no endocarditis stigmata or infectious symptoms. He was seen by Infectious Disease and Cardiology; the mass was stable on TTE. He was discharged with follow up.
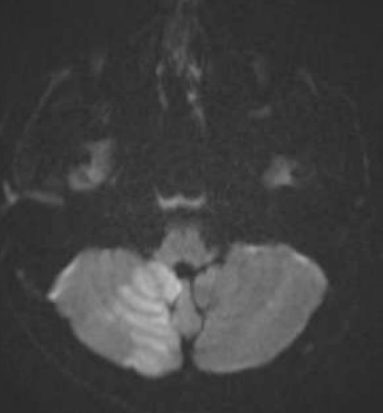
Two days later, he returned with right facial numbness and dysarthria and was found to have a right cerebellar stroke. TTE showed the mass to be larger and more mobile. A DNA sequencing culture from his prior admission was positive for Aspergillus. His B-1,3-D-glucan level was elevated. A CT chest showed nodular opacities consistent with fungal infection. An US of his right arm showed a septic abscess. He was diagnosed with Aspergillus endocarditis and valvulopathy with embolic features. He was started on micafungin and voriconazole. Due to induction failure, he was not a candidate for cardiovascular surgery. His B-1,3-D-glucan level downtrended. He sustained a second Left MCA stroke, emboli to his extremities, erosion of his pulmonary artery, and passed away three months after initial presentation.
Discussion: Fungal endocarditis can be an elusive diagnosis in patients at risk for thrombi, bacterial endocarditis or infiltrative processes that mimic infectious lesions. Fungal pathogens cause less than 2% of all endocarditis. Aspergillus is an aggressive pathogen responsible for 20-30% of all fungal endocarditis. It has a predilection for male, immunocompromised hosts with hematologic malignancies. Embolic phenomenon especially to brain, lungs and eyes, are present in most cases at initial presentation.
Diagnosis is difficult and diagnostic delays are common; 96% of blood cultures are negative in Aspergillus endocarditis. Echocardiography tends to show bulky vegetation. Modified Duke criteria exist for fungal endocarditis. Galactomannan, a component of the Aspergillus cell wall, and B-1,3-D-glucan, a non-specific fungal marker, can detect invasive disease in neutropenic patients. Definitive diagnosis requires tissue confirmation.
Treatment of Aspergillus endocarditis involves antifungal therapy with voriconazole and cardiovascular surgery including debridement. Often despite optimized surgical and medical interventions, the infection proves to be lethal. Chances of survival are 30-44% with surgical treatment, and without surgical intervention survival drops to 4% with antifungals alone.
Conclusions: Aspergillus endocarditis should be considered in immunocompromised patients with hematologic malignancy and a cardiac vegetation. Diagnosis requires specialized testing, and surgical treatment can increase survival in this otherwise almost universally fatal infection.