Background:
Teaching quality improvement (01} to house staff is still in its infancy. Using modified root cause analyses (RCAs) in monthly resident‐run conferences has been suggested as one manner to improve resident Ql exposure and skills. In a previously described patient safety curriculum, an internal medicine PGY3, supervised by a hospitalist. leads a modified RCA that focuses on a quality gap encountered on the teaching service. The types of interventions that result from such a conference has not been previously described. Better understanding of topics discussed in such conferences can help direct future 01 curriculum development and highlight opportunities for house staff.
Purpose:
To describe the nature and success of suggested interventions that were discussed in 18 recent resident‐run quality improvement conferences.
Description:
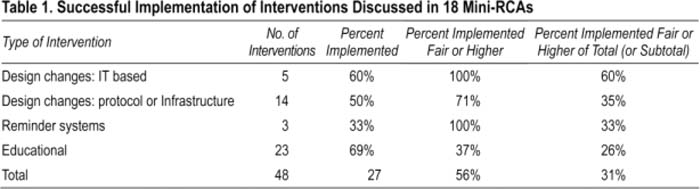
Individual cases for each QIC were presented monthly. After each QIC, chief residents and hospitalists agreed on the major interventions suggested in a moderated group discussion. In 18 conferences, 48 interventions were identified. These interventions were grouped into 4 broad categories based on a hierarchy of efficacy: educational, reminder systems, design changes (protocol or infrastructure), and design changes (IT based). Implementation status was tracked and the degree to which changes persisted over time was rated as poor, fair, good, or excellent. Cases included a lost guide wire during a code, incorrect medication or dosages, central line infections, missed diagnoses, disclosing errors, poor Transitions of care, and poor patient satisfaction. Of 48 interventions identified, 27 (56%) were implemented, but only 15 (31%) persisted in a meaningful way (defined as fair or higher persistence; Table 1). IT design changes, such as electronic medication reconciliation, were few but more likely to be successfully implemented (60%). Protocol design changes, such as mandating talk‐back for verbal orders or color coding DNR bracelets, though more commonly recommended were implemented less frequently (35%). The largest number of suggested interventions, 23, were of the educational type, and 16 of these suggestions were implemented. Persistence of these interventions was low, with only 37% showing fair or higher long‐term implementation success.
Conclusions:
Modified RCAs lead by house staff and moderated by hospitalists and chief residents, can lead to many interventions that persist in an organization. As expected, IT design changes were most often successfully implemented. Suggested educational interventions and protocol design changes were implemented less frequently and persisted less robustly. Future surveys of house staff, nurses, and other clinicians will assess whether this Ol program contributes to a culture of safety and quality.
Author Disclosure:
R, Jervis, none; E, Rule, none; K, Smith, none.