Background:
Hospital efficiency and throughput has a great impact on available bed‐days. When hospitals run at high capacity, the need to care for patients in the most efficient manner possible is of paramount importance to being able To accommodaTe the greatest number of patients. The ability for admitted patients to move as efficiently as possible through the ED may also be contingent on inpatient bed availability, particularly at certain times of day, when patients are more likely to be admitted. We identified the discharge process itself as an area where we might be able to gain efficiency.
Purpose:
Our goal was to reduce the time between placement of discharge orders and Ihe patient leaving the hospital room, releasing the bed to be cleaned.
Description:
We surveyed nursing staff to understand the factors that most affected their ability to discharge patients efficiently They considered their discharge‐related paperwork to require Ihe greatest amount of time. Based on their responses, we implemented 3 approaches to decrease Ihe lime between order placement and patient discharge. (1) We first designed a process through which discharge orders would print to Ihe ward clerk.
The ward clerk prioritized processing discharge orders over other work. (2) We updated the nursing discharge and medicine reconciliation note templates in our electronic medical record (EMR) so that they were prepopulaled with data already contained in the EMR. (3) Because documenting patient education is now an increasingly important part of the nursing discharge process, we created a “patient education note” that facilitated Ihe documentation required for common discharge diagnoses, pulling elements already present in the EMR. (4) We obtained unit‐level feedback weekly to reinforce our process in addition to determining if further changes needed to be implemented.
Conclusions:
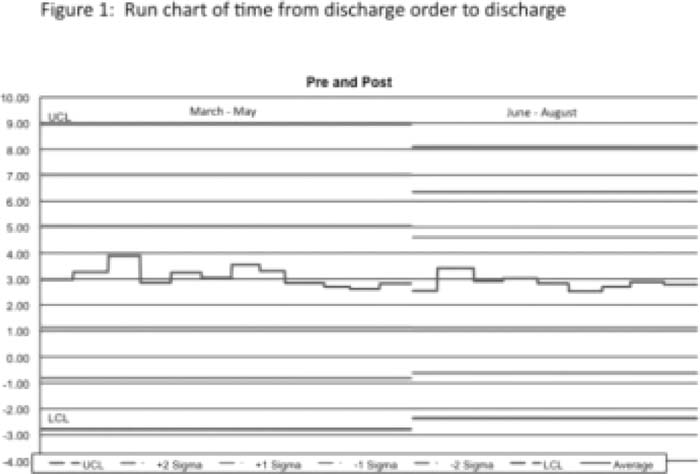
Prior to implementing this innovation, the time between order placement to bed release was 3.13 hours. This was decreased to 2.85 hours after the implementation of our new processes and templates, with less variability in the time required (Fig. 1). in addition to the potential ability to use the beds for newly admitted patients more rapidly, our intervention has improved satisfaction of the nursing staff by reducing their paperwork. We have not heard feedback that The ward clerk prioritizing discharge orders has led to delays in other orders being earned out. The use of EMR templates able to import information may be a generalizable way of reducing lime spent in paperwork or documentation of care processes, allowing care to be efficient.
Author Disclosure:
M. Johnson, none; L Dodge, none; M, A, Mote, none; L, Leykum, none.