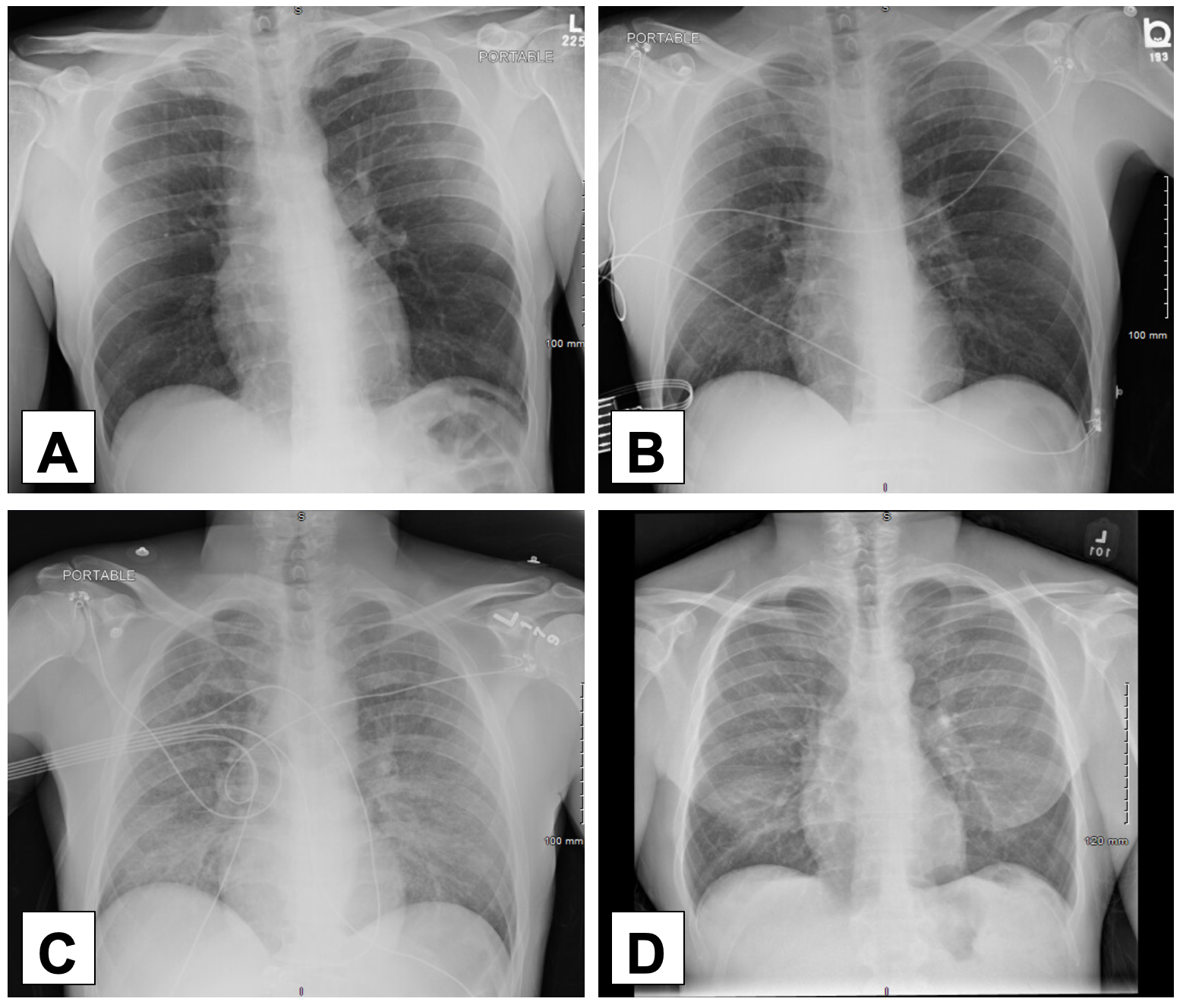
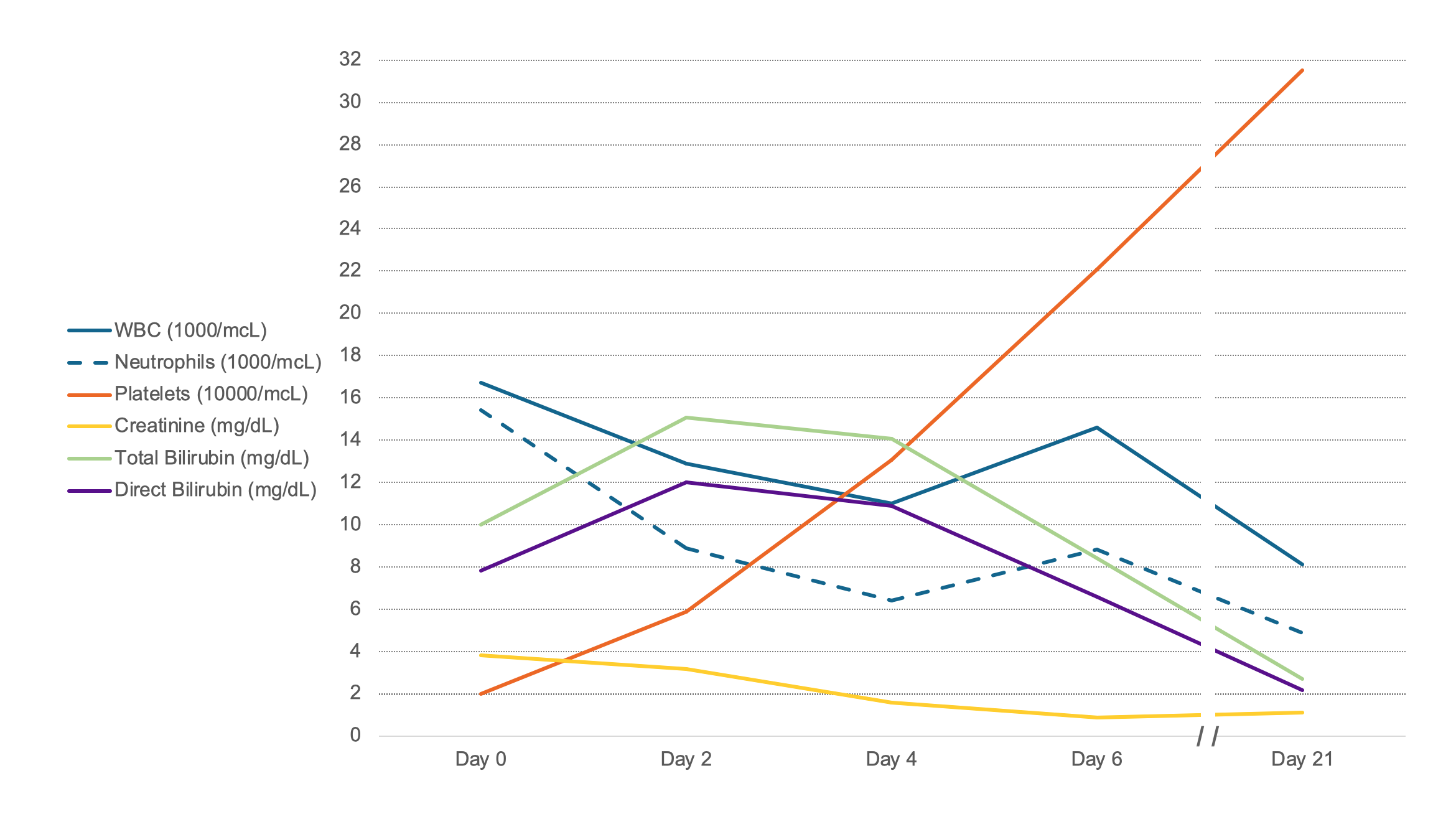
Case Presentation: A 46-year-old man presented with 1 week of fevers, chills, fatigue, myalgias, cough, hemoptysis, nausea, vomiting, diarrhea, and confusion. One month prior to presentation the patient started a new job performing sanitation and sewage work in basements. On presentation, he was afebrile, with pulse 98 and blood pressure 98/71. Exam was notable for icteric sclera, cervical adenopathy, abdominal tenderness, and bilateral lower extremity tenderness. Blood tests demonstrated WBC 16.7 with 92% neutrophils, platelets 19, creatinine 3.8, total bilirubin 10, CPK 1,067, lactic acid 2.5, and multiple low electrolytes. Imaging revealed diffuse pulmonary inflammation and mediastinal lymphadenopathy. He was started on broad-spectrum antibiotics for presumed sepsis and admitted to the hospital. All initial blood, urine, and stool culture data, as well as autoimmune workup, were negative. By day 5 his mental status and lab abnormalities had normalized and two days later his chest x-ray had cleared. Initial leptospirosis IgM antibodies were borderline during admission but later resulted as positive 2 weeks post-discharge.
Discussion: We present a case of Leptospirosis, or Weil’s disease, a rare condition primarily seen in tropical climates, first described in 1886 by Adolph Weil. Humans are exposed to Leptospira when in contact with animal urine as the spirochetes invade renal tubules. In urban communities this exposure if often associated with activities involving rats and rat urine. Clinically, patients with leptospirosis can present in two phases: anicteric or icteric. After 1-2 week incubation period patients may develop non-specific viral-like symptoms with headache, cough, shortness of breath, or abdominal pain. Indeed, our patient had presented to an emergency room 3 days into his illness with mild symptoms without jaundice and was presumed to have a viral illness and discharged home. Approximately 90% of these patients recover but a small percentage progress to the latter icteric phase with multi-organ inflammation, damage, and hemorrhage characterized by jaundice, rhabdomyolysis, renal failure, pulmonary hemorrhage, acute respiratory distress syndrome, and aseptic meningitis – all of which our patient demonstrated. Treatment includes penicillin group antibiotics or cephalosporins, though disease prevention via the identification of a patient’s exposure and reporting cases to health authorities are also important. IgM ELISA is often used for earliest detection.
Conclusions: Leptospirosis is extremely rare in developed countries but, due to changes in climate and human habitation, is an emerging disease with significant mortality. The patient presented initially with non-specific symptoms but then developed severe multi-organ damage requiring hospitalization. Antibiotics led to rapid improvement in all acute symptoms and lab abnormalities, allowing for strong support of this rare diagnosis.