Case Presentation: A 65 year-old woman with a history of renal cell cancer status post nephrectomy and breast cancer treated with lumpectomy and radiation presented with three weeks of progressive lower extremity weakness and confusion. She had poor short-term memory, word-finding difficulties, and difficulty walking. She had no fever, night sweats, or weight loss.
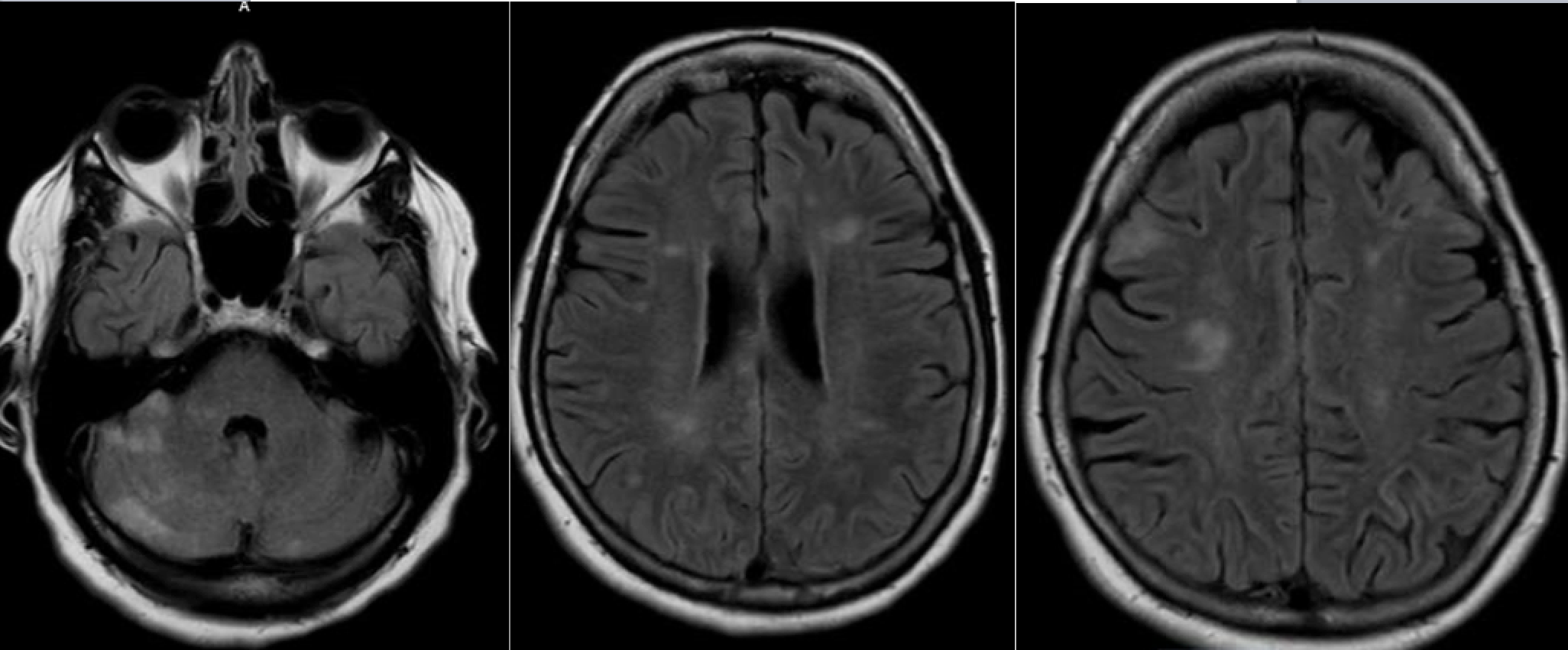
Exam was notable for disorientation, impaired memory, poor strength of the right lower extremity, diffuse hyperreflexia, and prominent dysmetria. Routine labs and a head CT were unremarkable. Brain MRI showed multiple intracranial lesions in the cerebrum and cerebellum with associated dural enhancement. Spine MRI was unremarkable.
Initial differential included malignancy versus embolic strokes. An EKG, echocardiogram, and telemetry monitoring were unremarkable. She underwent a lumbar puncture with CSF studies showing an elevated protein level and 7 WBCs. Cytology showed rare “atypical” cells but too few to characterize. Tumor markers and a paraneoplastic panel were negative. A whole body PET scan showed no evidence of a primary tumor or lymphadenopathy. A high volume lumbar puncture was repeated with no malignant cells seen on cytology. A repeat brain MRI ten days after her initial scan was concerning for evolution of embolic infarcts, therefore a transesophageal echo was obtained which was negative for a thrombus or vegetation.
Clinically she worsened with progressive inability to move bilateral lower extremities, and degrading mental status. CNS vasculitis was considered in consultation with rheumatology. Neurosurgery expedited an urgent brain biopsy and she was started on high dose solumedrol. Pathology revealed findings consistent with intravascular large cell lymphoma. Urgent chemotherapy was initiated with rituximab, cyclophosphomide, doxorubicin, vincristine, and prednisone (R-CHOP) and high dose methotrexate with improvement of her neurological status.
Discussion: Intravascular large cell lymphoma (IVL) is a rare subtype of large cell lymphoma that is notable for proliferation of lymphoma cells within small blood vessels of affected organs with relative sparing of the surrounding tissue, and without an extravascular tumor or mass. Any organ system may be affected, but the central nervous system and skin are most commonly involved. Patients with CNS involvement may present with focal sensory or motor deficits, weakness, altered sensorium, seizures, and rapidly progressive dementia. Blood work may reveal an elevated LDH and high inflammatory markers. Absence of lymphoma cells in the peripheral blood, lymph nodes and reticuloendothelial system is a hallmark. There are no pathognomonic imaging findings, however it may mimic CNS vasculitis. IVL of the CNS can also imitate a stroke, encephalitis, multiple sclerosis, or even brain metastases. Timely acquisition of a surgical specimen of the affected organ is key to diagnosis as it is often fatal.
Treatment includes systemic chemotherapy and CNS directed treatment, most typically R-CHOP and high dose methotrexate. Prognosis is quite poor. Historically this diagnosis was made post-mortem, but with treatment, three year survival rates can be up to 30%.
Conclusions: Intravascular lymphoma of the CNS is a rare condition that mimics many neurological conditions such as stroke, vasculitis, and cancer. To ensure a correct and timely diagnosis, the hospitalist should pursue an invasive brain biopsy if a patient with multiple brain lesions clinically worsens despite a thorough evaluation.