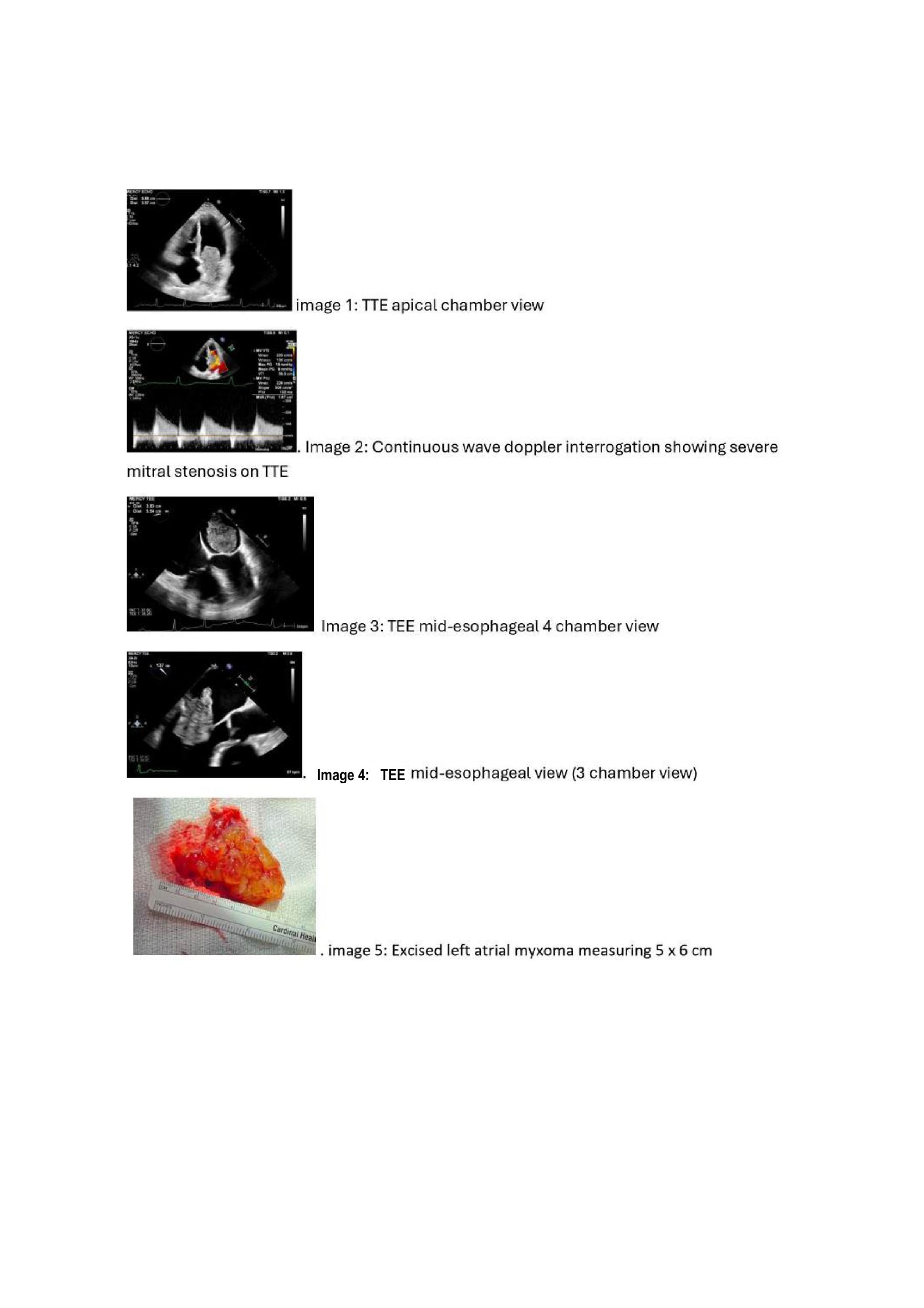
Case Presentation: A 65-year-old male was admitted with COPD exacerbation. Imaging studies showed advanced emphysematous changes and cardiomegaly. He was found to be in newly detected atrial fibrillation for which a transthoracic echocardiogram (TTE) was obtained. TTE revealed a moderately dilated left atrium (LA) with a large, highly mobile mass (6.8 x 3.5 cm) prolapsing into the mitral orifice, causing moderate to severe mitral stenosis with a mean gradient of 7 mmHg; suggestive of obstruction severity. The right ventricle was mildly dilated with low normal systolic function, and there was moderate tricuspid regurgitation with an estimated right ventricular systolic pressure of 45 mmHg [Image 1-2]. Cardiology was consulted and further evaluation with transesophageal echocardiography (TEE) confirmed the presence of a large, gelatinous LA mass with a stalk originating near the coronary sinus. The mass was highly mobile and posed a significant risk of embolization [Image 4]. The LA mass was consistent with myxoma, a primary cardiac tumor, necessitating urgent surgical intervention. The patient underwent an urgent conventional sternotomy with cardiopulmonary bypass and an LA mass, measuring 5 x 6 cm, was excised with a good margin from its attachment site [Image 5], and the defect was closed with a bovine pericardium patch. Additionally, a bi-atrial Maze ablation with left atrial appendage clipping was done. The surgery was completed successfully with no intraoperative or postoperative complications. The patient recovered well and was discharged on postoperative day 4.
Discussion: The 2023 American College of Cardiology (ACC) guidelines provide a Class I recommendation for TTE in patients with newly detected atrial fibrillation (AF). TTE is essential for evaluating cardiac structure, assessing stroke and bleeding risk factors, and identifying underlying conditions that inform subsequent management strategies. This case highlights the critical importance of performing TTE in evaluating new-onset AF, even when a common precipitant, such as a COPD exacerbation, is present. Relying solely on an apparent trigger risks overlooking underlying structural abnormalities that are easily identifiable with this readily available diagnostic tool. Atrial myxomas, although rare and benign, can lead to severe complications, including systemic embolization or hemodynamic instability. In this case, the incidental detection of a large, highly mobile myxoma during routine TTE likely prevented a potentially life-threatening embolic event.
Conclusions: AF poses a significant burden in patients with chronic obstructive pulmonary disease (COPD), with studies reporting a prevalence of 20.58%, especially during exacerbations. This case emphasizes the importance of performing TTE in such populations to exclude structural heart disease. Routine use of echocardiography in these patients is not merely guideline-driven but also potentially lifesaving, as demonstrated by this case. Early recognition of structural abnormalities such as cardiac myxomas enables timely intervention and optimal patient outcomes.