Background: Medicine procedure services (MPS) have been shown to increase Internal Medicine (IM) procedure volume, procedure completion rates, adherence to best practice safety measures, resident involvement, and resident satisfaction. However, deployment of MPS can be challenging as it requires significant lead time for ensuring skillset consistency, provider scheduling, and developing referral sources. At the same time, long-stay patients (LSP) are increasingly common in acute care hospitals, and their low acuity presents a barrier to service line development and innovation due to the cost of staffing.
Purpose: We perceived an opportunity to create a sustainable care model by merging an existing LSP service with a nascent MPS using core faculty. The MPS was designed as a hybrid service with financial and operational sustainability, with the goal of providing sufficient lead time to onboard faculty, build skillsets, and develop a steady revenue stream for procedures. A secondary goal was to improve continuity in the care of LSPs and obviate need for moonlighting.
Description: In July 2020, the MPS was implemented, tied to two existing service lines: First, MPS assumed responsibility for the LSP service, previously staffed by rotating moonlighters; second, MPS coordinated procedure requests with pre-selected IM residents covering inpatient wards. This hybrid ensured both stable patient encounters (via LSP service) and adequate bandwidth for procedures (via IM residents). The IM residents’ attending was also credentialed for procedures and served as backup in case of MPS faculty illness. The core faculty model provided continuity for LSPs and a consistent skillset for procedures (arterial line placement, arthrocentesis, central line placement, lumbar puncture, paracentesis, thoracentesis, thrombolytic instillation, ultrasonography of lung). MPS faculty were oriented to standardized workflows and relevant documentation and billing requirements. The workflow included performing consultations by standard template for all inpatients and outpatients and seeing all inpatients on post-procedure day 1 to assess for complications and ascertain additional needs. Growth in procedure volume and revenue was facilitated via education, workflow enhancement, and cultivation of alternative referral sources. Education was provided to faculty and residents by email, Division meetings, and a procedure-focused Journal Club. Workflow was facilitated by amending existing procedural care pathways and creation of an electronic order for procedure requests. Referral sources developed included Emergency Department (ED, via a care pathway focused on avoiding unnecessary admissions and delays), Cancer Center (to minimize the need for urgent IR referrals and ED visits), and other outpatient care areas. As volume increased, an elective experience on MPS was added to our Advanced Practice Fellowship in Hospital Medicine, which provided additional bandwidth and educational enrichment.
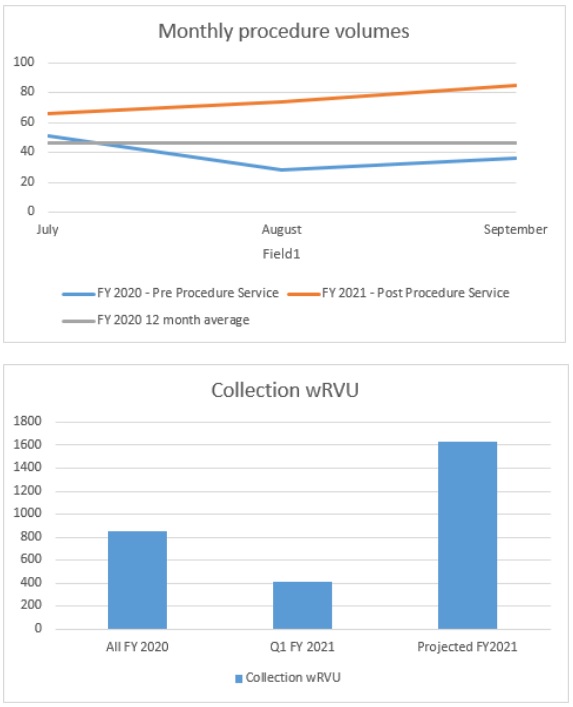
Conclusions: Implementation of an MPS linked to a LSP service led to increased procedure volume and collection wRVU (graphs), improved long-stay patient-provider continuity (5 providers compared to 27), obviated moonlighting (0% compared to 100%), and provided a sustainable platform for growth and innovation.