Background: D-dimer is one of the most commonly used tests because of its high sensitivity, but a high false positive rate prevents healthcare providers from efficiently diagnosing pulmonary embolism (PE). This leads to many patients unnecessarily undergoing CT pulmonary angiography (CTPA) scans in the emergency department (ED). This study sought to determine if there is a better way to use the d-dimer test to diagnose PE. We wanted to create a prediction model that more effectively risk stratifies patients presenting with concern for PE.
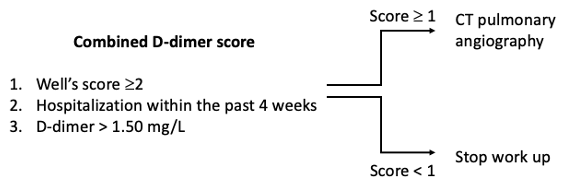
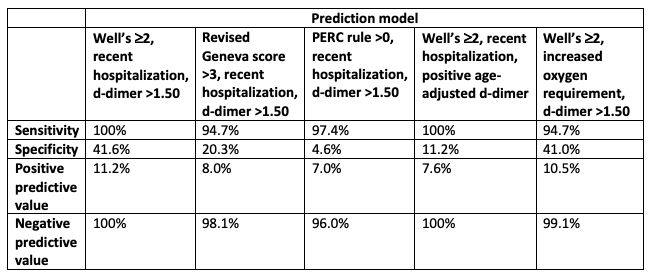
Methods: We conducted a retrospective review of 555 patients who underwent CTPA and d-dimer testing in the ED to determine an algorithm for predicting PE. When comparing d-dimer cutoff values, we found that a d-dimer cutoff of 1.50 mg/L had the highest accuracy but a sensitivity of 76.3%, leading to many missed diagnoses. Both age-adjusted and the standard d-dimer cutoff of 0.50 mg/L were highly sensitive tests but have low specificity. We then analyzed multiple predictors in different combinations from a patient’s history, physical exam and risk scores. One such prediction model is the d-dimer prediction model which is positive with a d-dimer >1.50 mg/L or a Wells’ score greater than or equal to 2 or hospitalization within 4 weeks.
Results: With the d-dimer prediction model, sensitivity improved to 100% and specificity improved to 41.6%. Including the risk factor of recent hospitalization includes many patients who would be missed by d-dimer or Wells’ score alone. Other combinations using the revised Geneva score, PERC rule, age-adjusted d-dimer and increased oxygen requirement did not perform as well in discriminating PE from other diagnoses.
Conclusions: In our study, the novel d-dimer prediction model resulted in a 32.4% reduction in false positive results and could reduce in the number of CT scans that are ordered in the ED. Applying this to our hospital system for one year, there is a $896,354 reduction in healthcare costs while also avoiding side effects of CTPA in 398 patients such as contrast reactions, kidney injury and radiation exposure. In conclusion, the d-dimer prediction model could greatly improve precision when diagnosing PE in the ED.