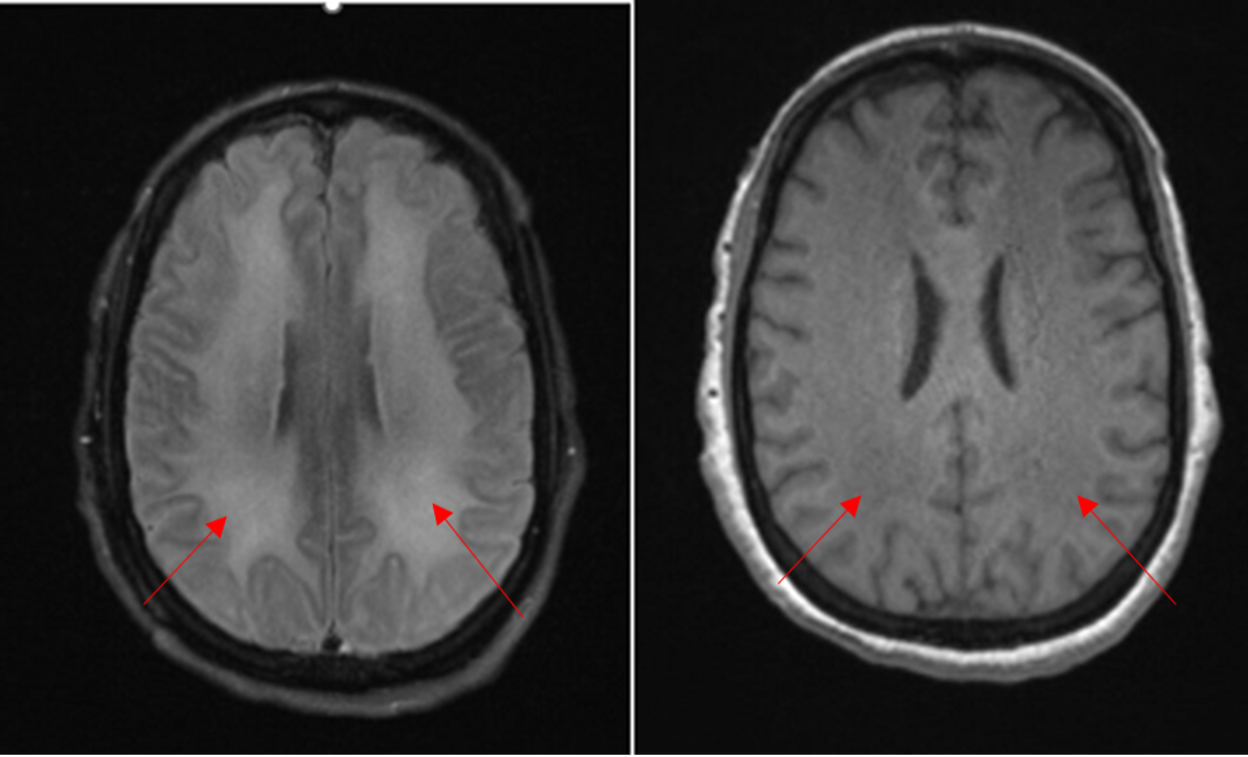
Case Presentation: A 48-year-old woman with history of anxiety, depression, chronic pain, and polysubstance abuse was brought to the hospital for unusual behavior. She was hospitalized one month prior for behavior change and diagnosed with substance induced psychosis. She returned to the hospital after two weeks of recurrent bizarre behavior at home including wandering disrobed, illogical answers to questions, and homicidal ideation. Neurologic exam was non-focal. Select lab data: Urine tox screen positive for cocaine and cannabis. TSH, B12 levels normal. CRP < 0.4 mg/L, ANA negative. CSF: 1 WBC, 0 RBC, prot 37 mg/dL, CSF IgG Index 1:1, encephalopathy panel negative. The initial leading diagnosis was again substance induced psychosis, though we also considered autoimmune encephalitis and metabolic causes. Psychiatry and neurology consulted. The patient’s behavior did not improve over three weeks with trials of anti-psychotics and benzodiazepines. Lumbar puncture revealed oligoclonal bands with an IgG index of 1:1, suggesting intrathecal IgG synthesis, though encephalopathy panel was negative. Subsequent MRI showed signs of diffuse leukodystrophy (Fig 1), raising concern for a toxic or autoimmune process. The imaging results of diffuse leukoencephalopathy in combination with elevated IgG index was consistent with a diagnosis of levamisole-associated multifocal inflammatory encephalopathy (LAMIE) from levamisole-adulterated cocaine use. There were extensive white matter changes seen on MRI, indicating poor overall prognosis. She was given an empiric trial of neuromodulation with IV methylprednisolone for 5 days. Her symptoms were treated with lorazepam, divalproex, and risperidone. While there was modest reduction in her agitation and impulsivity, her condition did not significantly improve and she was discharged to her family’s care.
Discussion: Hospitalists should be familiar with toxic effects of levamisole, a common adulterant of cocaine. While agranulocytosis and cutaneous vasculitis have been well described, a number of recent case reports have described LAMIE. LAMIE is an immune mediated process that causes CNS demyelination, similar in presentation to multiple sclerosis or acute disseminated encephalomyelitis (ADEM). It is characterized by MRI findings with multiple asymmetric white matter lesions, mostly in the periventricular areas. CSF can show pleocytosis, elevated IgG index, or oligoclonal bands, as in our case. A history of cocaine use or positive urine toxicology can distinguish from other etiologies. While there are not clear treatment guidelines, it is treated similarly to other autoimmune disorders with high dose IV steroids. It is also critical that cocaine use, and thus levamisole exposure, is discontinued. While prior case reports have shown favorable prognostic outcomes, our patient unfortunately did not improve. Her prior diagnosis of substance induced psychosis likely delayed her definitive diagnosis of LAMIE and subsequent treatment.
Conclusions: Our patient was diagnosed with LAMIE based on history of cocaine use in setting of characteristic MRI and CSF findings. While uncommon, LAMIE should be considered in patients with persistent neurologic and psychiatric symptoms in the setting of cocaine use. Prompt diagnosis is critical for appropriate interventions.