Background: The merging of academic and community hospitals into a single large healthcare system often does not account for the differences in health care delivery between sites, despite attempts by the system to streamline care through standardized policies, common metrics, and a shared medical record system. Multi-site service lines can be an effective strategy for reducing this fragmentation but only with clear goals and sufficient resourcing. Unfortunately, because high cost services such as the surgical specialties are usually the primary focus for service-line restructuring, hospital medicine may not be as well-funded. To promote self-governance and to create alignment, we elected to form a hospitalist-led multi-site coalition.
Purpose: To create a hospital medicine service line leadership team that would effectively address common acute care issues through goal alignment, reduction of variability, standardization of policies and informatics.
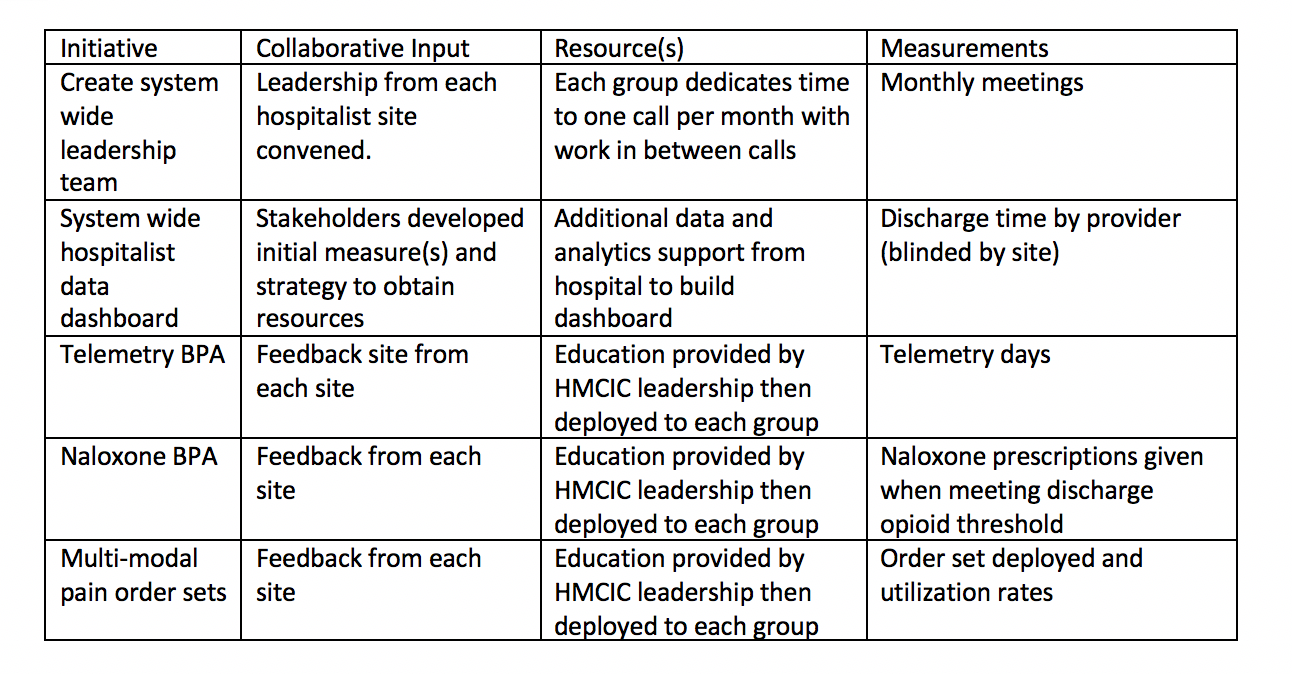
Description: In April 2018, hospitalist leaders across a large healthcare system formed the Hospital Medicine Clinical Innovation Collaborative (HMCIC). The HMCIC represents academic hospitalists, health-system employed hospitalists and an independently contracted group composed of 41 physicians who together form the hospitalist workforce for 11 community hospitals and 1 academic teaching hospital. The HMCIC meets on a monthly basis via teleconference and is comprised of leadership from each of the system hospitals, hospital medicine quality directors, a project manager, and a data analyst. Agenda items focus on issues common to all sites, such as informatics related problems, system-wide quality improvement initiatives, and shared difficulties such as geographic rounding or multi-site care plans for certain complex patients. System-wide outcomes metrics, such as length of stay and readmissions, and transparency of data collection and outcomes, are also regularly discussed. Meetings additionally include brainstorming sessions on ways to improve alignment, increase resources and reduce variability in care delivery. Since inception, the HMCIC has collaborated on multiple initiatives, including development of a provider level discharge tool, which allows each site to obtain provider-level data on discharges before 11am, a virtual sepsis monitoring system, coding best practices, the deployment of a ‘Telemetry BPA’, One key initiative was the formation of the Medicine Order Set Standardization Team (MOSST), a hospitalist-led group intended to align conflicting hospital orders sets in the Epic Electronic Health Record into a single system-wide order set. Reduction of opioid usage in the inpatient setting has also been a focus of the HMCIC, leading to two further projects: a multi-modal pain order set and an automated naloxone prescription (Table 1). Each one of these initiatives is paired by measurable outcomes to gauge success for system leadership.
Conclusions: A provider-led hospital medicine leadership team can be an effective strategy for promoting system unity around common issues such as standardized order sets and opioid reduction. Through collaboration and shared goals, hospitalist groups working in conjunction within a health care system can have a large impact on value-based care and can be a powerful voice for system-wide change.