Background:
Cardiac biomarkers, such as myoglobin and B-type natriuretic peptide (BNP), are frequently ordered in the emergency room and inpatient settings. Newer studies and guidelines have called into question the value of these tests in diagnosis and management. Myoglobin is commonly used for early diagnosis of acute coronary syndrome (ACS) in patients who present with chest pain, yet the 2014 American Heart Association/American College of Cardiology (AHA/ACC) guidelines state that myoglobin is no longer useful in the diagnosis of ACS given the improvement in modern troponin assays. BNPs are frequently ordered in the emergency room by both Emergency Medicine (EM) and admitting providers, even when the diagnosis of heart failure (HF) exacerbation is already certain. The 2013 AHA/ACC guidelines state that BNP is most useful for diagnosis of HF exacerbation when the diagnosis is in doubt. Additionally, although BNP yields prognostic information, it is not clear how useful BNP is in guiding management of acute decompensated HF.
Purpose:
Our goal was to decrease inappropriate use of myoglobin and BNP according to evidence based guidelines in an effort to control cost without affecting diagnostic sensitivity.
Description:
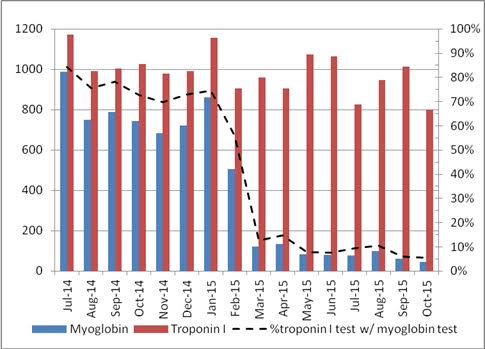
At a community teaching hospital we assembled a multidisciplinary team with members from Hospital Medicine, Cardiology, EM, and Laboratory Medicine to improve ordering of cardiac biomarkers. The vast majority of myoglobin tests at our institution were ordered via a myoglobin/troponin panel that contained an order for both tests in our electronic health record (EHR). Our team eliminated this panel from the EHR used in our Emergency Department (ED) and from the separate EHR that is used in the inpatient setting while still allowing both tests to be ordered separately. With the elimination of the myoglobin/troponin panel there was an immediate 84% reduction in the number of myoglobin orders (Figure). With an additional educational campaign we have sustained a cumulative 91% reduction in myoglobin orders from the original baseline. The majority of BNPs at our institution are ordered by EM and Internal Medicine (IM) providers while their patient is in the emergency room. We launched an educational campaign on appropriate use of BNP, after which we saw a 28% reduction in BNP orders. After implementation of an electronic alert in the ED EHR we saw a cumulative 57% reduction in BNP orders from the original baseline. These reductions have resulted in a combined savings of over $200,000 per year in direct costs to our institution.
Conclusions:
Simple educational and systems interventions may have a dramatic impact on cardiac biomarker ordering and lead to substantial cost savings.