Background: The inpatient acute care environment has faced increasing capacity constraints since the COVID-19 pandemic. Factors like deferred care, nursing shortages, and a sicker population contribute to these constraints. Many systems have sought to improve patient flow to alleviate these issues. Efficient patient movement through care steps enhances patient satisfaction, reduces stay length, and minimizes the risk of adverse events. Quality improvements, especially in patient populations with conditions like sepsis, acute coronary syndrome, and transplant, can be significant as they require rapid condition recognition and prompt treatment. Incorporating standardization of care, viewed through a LEAN methodology lens, can smooth patient flow and reduce time waste.
Purpose: This proof-of-concept pilot aimed to develop a process utilizing electronic health record data and natural language processing to identify and historically benchmark sepsis care milestones. The focus was on reducing variability in patient care processes and improving care standardization for sepsis patients. Long-term goals include extending these methods to other patient populations.
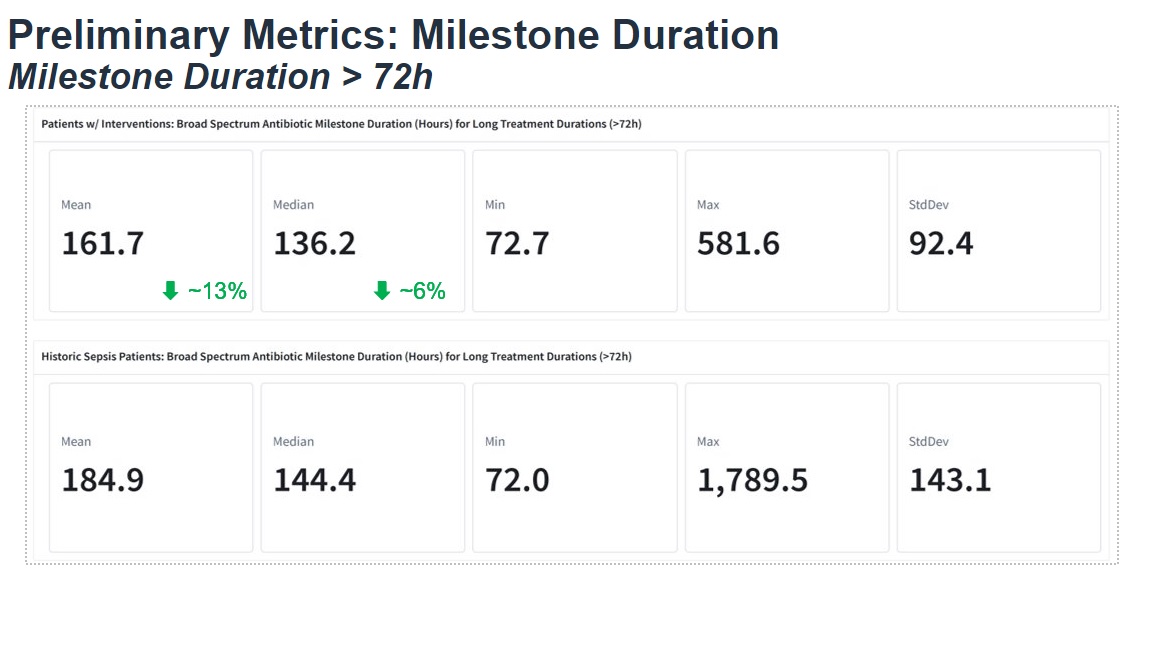
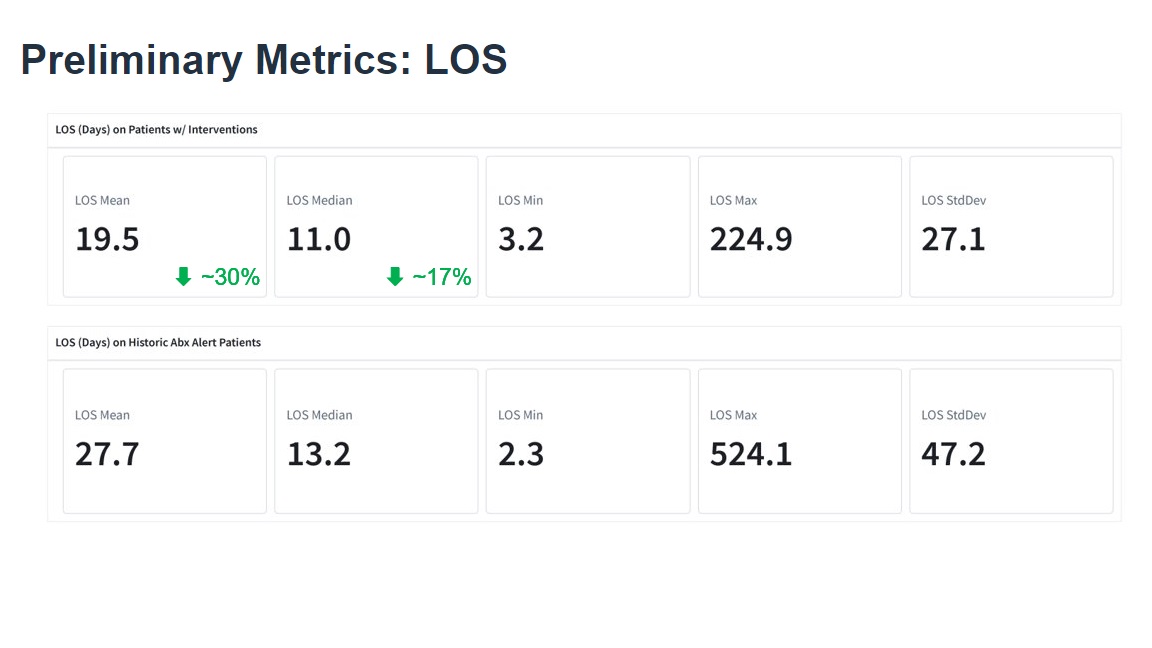
Description: We partnered with Palantir Technologies to create this solution using the Foundry platform. A multidisciplinary team identified various treatment milestones occurring outside of the CMS sepsis treatment bundle. Initial milestones included physical therapy, case management, and infectious disease consults as well as antibiotic de-escalation strategies, and time to imaging and labs. The pilot milestone for alert build was antibiotic de-escalation for patients on broad-spectrum antibiotics for over 72 hours. An alert system was developed that signaled to the antimicrobial stewardship (ASP) team for antibiotic review. If deemed appropriate, the ASP team contacted the physician to discuss de-escalation, reduced duration or discontinuation of broad-spectrum antibiotics at the time of the alert. The pilot went live in March of 2023.Baseline statistics for the index population of 3651 sepsis patients were gathered and included a mean length of stay of 27.7 days, and a mean time on broad spectrum antibiotics of 184.9 hours. The first version of the alert went live March of 2023 and fired an average of 30 times weekly. Forty percent of alerts have led to de-escalation of antibiotics while thirty two percent of alerts have led to a duration reduction or discontinuation of antibiotics. Metrics for the alert intervention population have shown a reduction in mean length of stay to 19.5 days (30% reduction), and a mean time on broad spectrum antibiotics of 161.7 hours (13% reduction).
Conclusions: The project demonstrates the potential of using historically benchmarked milestones in combination with AI technology to improve patient flow and treatment efficiency. The success of the pilot suggests a scalable model for enhancing patient care in various populations. While not a direct focus of this pilot program, reductions in length of stay and improvements in antimicrobial stewardship can lead to reduced antimicrobial resistance, and a reduced risk of adverse events in addition to cost savings and improved bed capacity. In addition to expansion of milestones and alerts, future work will look at adding automation to the alert build process and leveraging large language models for unearthing insights on milestones with historical variability.