Background: Over the course of several months, five adolescent patients were admitted to the hospital after intentional self-injurious behaviors involving foreign body ingestion. These patients were previously living in residential treatment centers, and via social media alerted each other of the benefits of being admitted to a children’s hospital including: private rooms/bathrooms, individualized attention, attendance at Child Life events, and an overall sense of a more nurturing environment. Once cleared medically for transfer back to the facilities, the patients ingested objects found either within the hospital rooms or on the hospital unit, prolonging the hospital length of stay. After discharge, many patients were quickly readmitted following repeat ingestions, citing the secondary gains of being in a children’s hospital.
Purpose: The growing number of patients with psychiatric conditions or at-risk behaviors being admitted to children’s hospitals is a nationwide problem. These patients place themselves and staff at risk, particularly in an environment not accustomed to caring for their unpredictable behavior. At our institution, self-injurious acts escalated in some patients. One staff member sustained a serious injury while trying to redirect the patient. All caregivers faced the dilemma of providing appropriate care for these patients while maintaining their own safety and well-being.
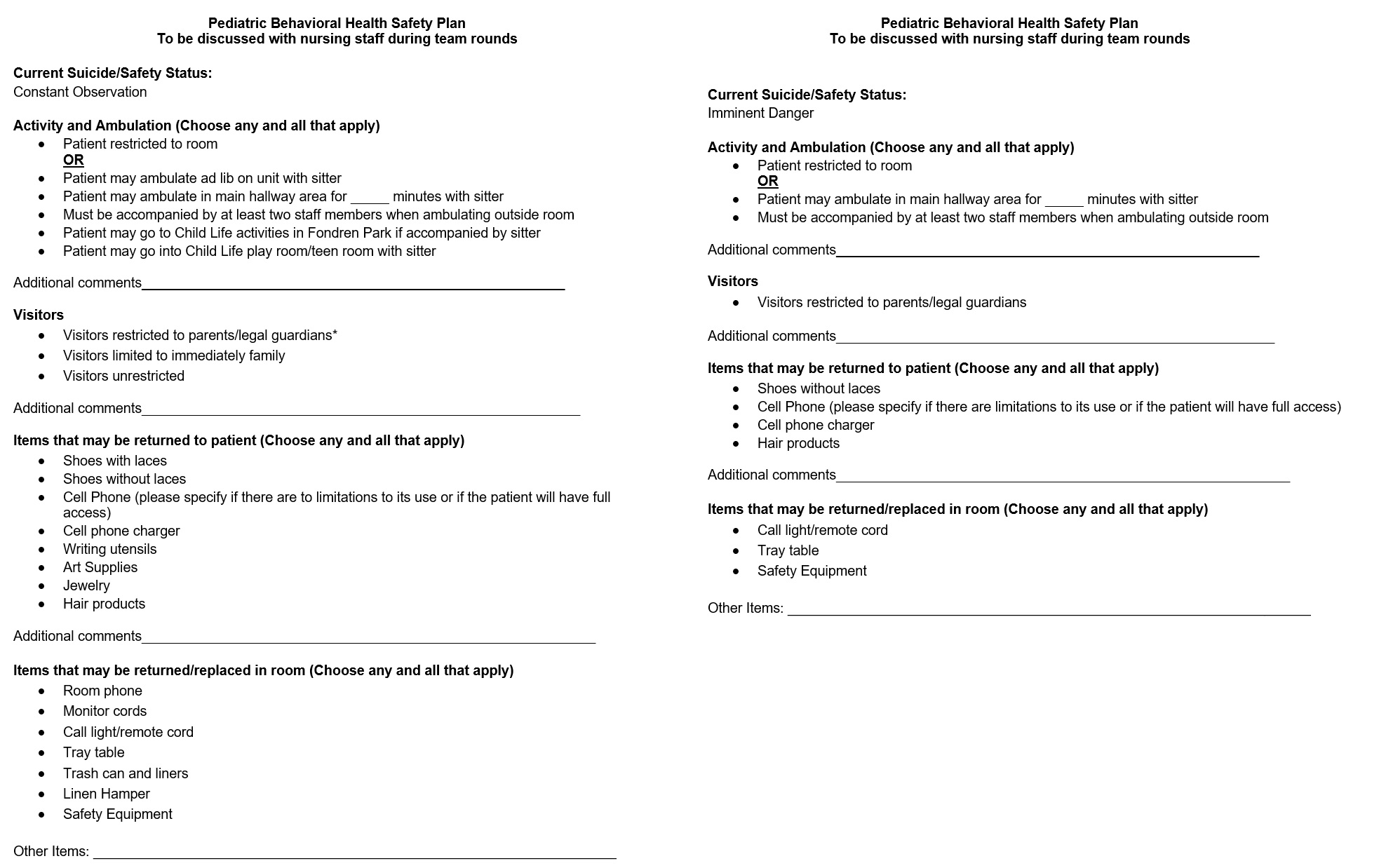
Description: In response to these events, our hospital created a multidisciplinary group consisting of: Pediatric Hospitalists, Pediatric Psychiatry, Nursing, Child Life, Security, Maintenance, and Food Services. Over the course of six months, this group created several response plans that could be implemented at any time during an admission. Patients identified with behavioral health concerns were stratified into different risk categories – “Constant Observation” vs. “Imminent Danger”. The risk assignment dictated resources that would be available to them, as well as protocols and behaviors that staff must follow. Additionally, an order set was created for use in our electronic medical record to assist in urgently ordering psychiatric medications.
Conclusions: Patients with behavioral health issues are a rapidly growing population in children’s hospitals nationwide. In addition to a multidisciplinary approach, formalized policies and procedures are essential to providing consistent and targeted care. The policies created at our institution in response to a subset of at-risk patients, have now been generalized for use in any patient with behavioral health concerns, resulting in improved patient care and staff well-being.