Background: Medication alerts are one of the touted safety features with the electronic health record (EHR). With time, users tend to override the alerts, which leads to patient harm. The phenomenon of “alert fatigue” is well known to any practicing clinician. Frequent interruptions of little value train physicians to disregard alerts in favor of efficiency. Prior to the described innovation, our organization had 1.01 medication alerts per medication ordered. An alert no longer functions as an “alert” if it fires every time a provider signs an order. This alarming rate served as the stimulus to form a multidisciplinary team to manage medication alerts.
Purpose: The multidisciplinary, “Drug Alerts Subcommittee,” was tasked to oversee medication alerts in our organization. The goals were to modify existing alerts and create new alerts to improve patient safety while simultaneously reducing alert fatigue.
Description: Our institution currently uses Epic health record and subscribes to First Databank for medication alerts. To address our high alert rate, the Pharmacy & Therapeutics (P&T) Committee supported creation of a Drug Alert Subcommittee. We incorporated advice from our legal department in the creation of the subcommittee. This team reviews alerts and recommends methods in modifying the alerts to improve patient care. These recommendations are presented to P&T for final approval.
This team is comprised of representatives from multiple areas and disciplines. We include physician informaticists, inpatient and outpatient pharmacists, pharmacy information technology (IT) specialists, a medication safety officer, and physicians representing inpatient, emergency, and outpatient departments.
We use reports from our EHR to identify high frequency alerts that also have high override rates. Instead of a simple, binary approach to drug alerts with an “on or off” strategy, we employee an arsenal of strategies to improve alert specificity. Our multidisciplinary team brainstorms ideas and proposes solutions such as changing the alert severity level, modifying the types of medications involved in the alert, increasing allowances for duplicate therapy alerts, suppressing alerts within an order set, or suggesting a more creative decision-support solution.
In keeping with the subcommittee’s mission to improve safety, the team also serves to create alerts based on institution events and Institution of Safe Medication Practices (ISMP) reports.
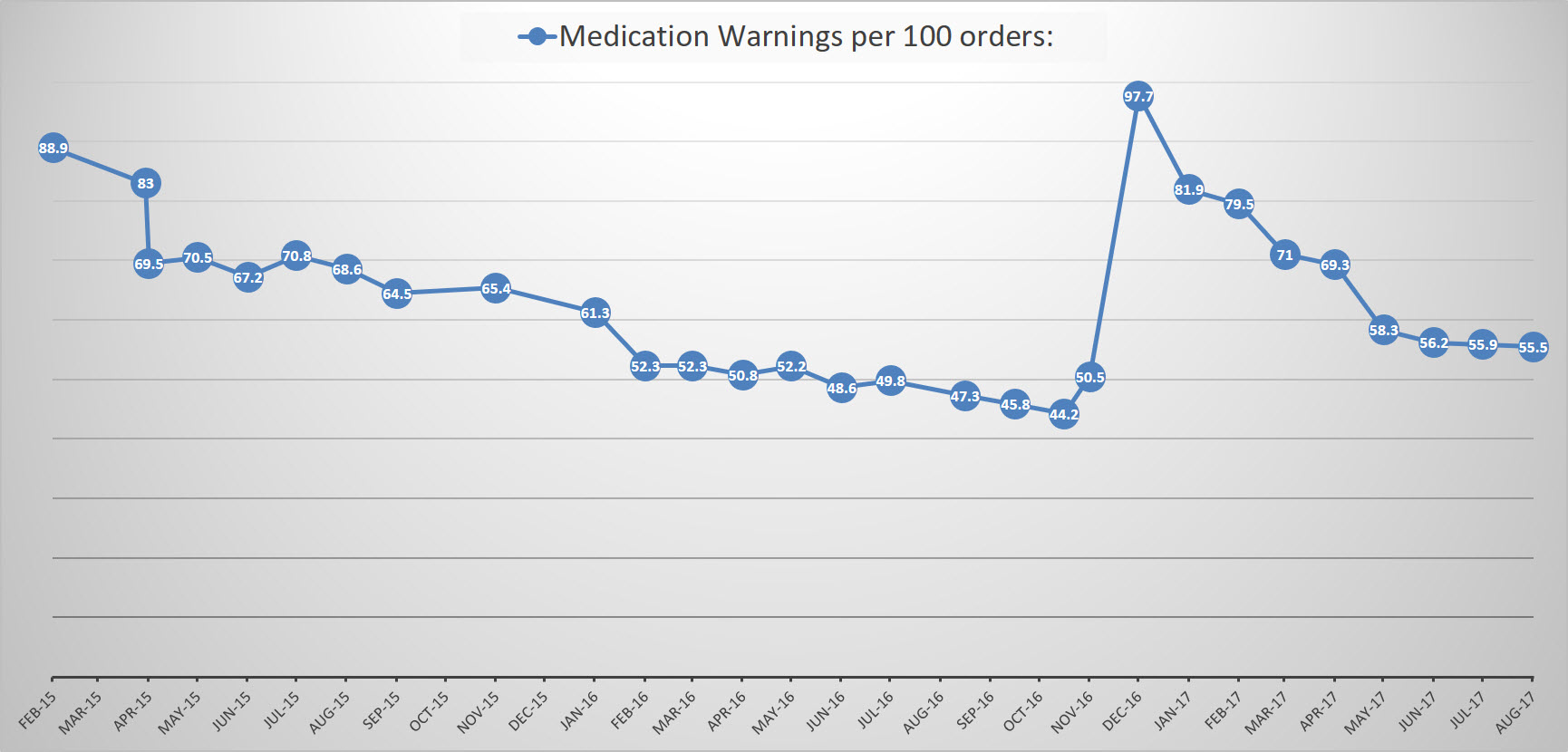
Conclusions: With a well-designed strategy, our institution brought together the appropriate leaders to help reduce our medication alert rate from 88.9 alerts per 100 medication orders when the committee first started to 55.5 alerts per 100 medication alerts. This amounts to a reduction in ~108,000 alerts each month. And most importantly, this was accomplished without identifying a single related adverse medication event. This decrease in alerts represents a large improvement in the specificity of alerts and therefore, an improvement in physician and pharmacist alert fatigue. The optimal number of alerts is not yet defined, but the drug alerts subcommittee continues to work towards improving patient safety and improving physician and pharmacist interactions with the EHR by strategically improving the specificity of medication alerts.