Background: The US Bureau of Labor Statistics estimates that healthcare workers experience workplace violence at 4 times the national average and providing care to patients with decompensated psychiatric illnesses disproportionately increases the risk of workplace assault (1). 20-40% of hospitalized medical patients have comorbid, decompensated psychiatric conditions that can impair insight regarding chronic medical conditions, decrease compliance with medical plans of care, and contribute to poor clinical outcomes (2). We sought to understand the effects of a new physical unit and a revamped workflow on patient outcomes and staff safety.
Methods: We performed a retrospective analysis of patients treated on our medicine – psychiatry collaborative unit of an 882-bed academic safety net hospital from January 15, 2015 to January 14, 2017. Baseline data was collected January 2015 to August 2015. The structural intervention, in August 2015, consisted of single-bed rooms and adjacent staff workspaces secured from patient areas, all secured from the remainder of the hospital. On January 15, 2016 the re-engineered care model and process intervention was implemented. Nurses received Satori Alternatives to Managing Aggression (SAMA) training, a behavioral emergency response team was implemented, and hospitalists, psychiatrists, therapists and unit social workers co-rounded daily and actively participated in discharge planning.Poisson regression was performed to determine differences between safety, clinical and operational metrics comparing the baseline period to the structural intervention period, the process intervention period and the structural with process intervention period. A p-value of <0.05 was considered significant.
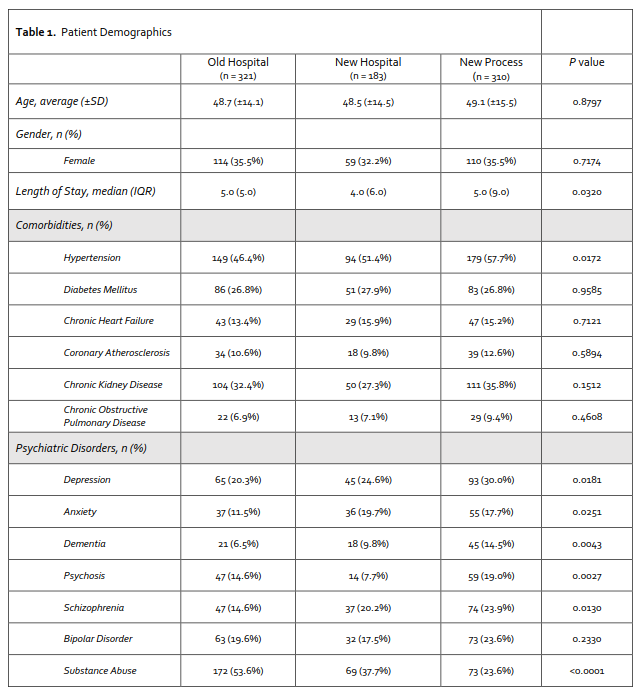
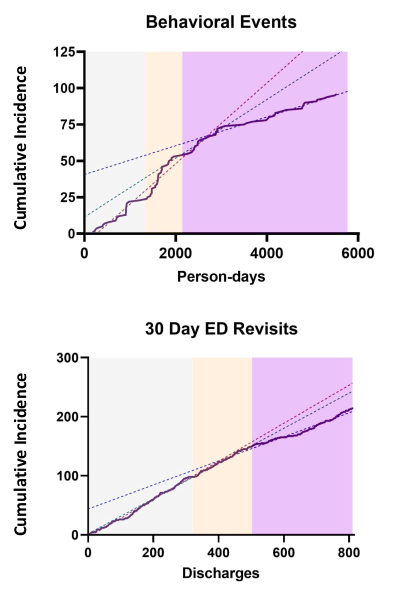
Results: The primary analysis identified 321 pre-intervention, 183 post-structural intervention, and 310 post-process intervention discharges. Patient age, gender, and medical comorbidity were statistically similar in all domains except for hypertension. Substance use disorder was higher in the pre-intervention cohort while depression, acute psychosis, anxiety disorders, and dementia were more prevalent in the post-structural and post-process intervention periods. (Table).The structural intervention did not change the frequency of workplace violence. Physical assaults occurring before and after the process intervention found a relative risk reduction (RRR)of 2.0 (95% CI 0.28 to 0.91, p = 0.021). A RRR of 2.5 (95% CI 0.25 to 0.75, p = 0.0128) was noted when comparing the pre-intervention and the post-process change period (Figure).The rate of emergency department utilization at 30 days post discharge was 30.5 % pre-intervention, 27.9% after the structural intervention (p= 0.588), and 21.0% after the process intervention (p=0.089 vs structural, p= 0.015 vs baseline) (Figure).There was no difference in falls or length of stay between baseline, structural, process and structural plus process periods.
Conclusions: We sought to evaluate the separate and cumulative impacts of structural and process changes on the safety, operations and clinical care of patients on a medicine-psychiatry collaborative unit. Our results suggest that the incidence of workplace violence and the rate of emergency department utilization after discharge, can be meaningfully and summatively improved by changes to both the physical environment and workflows of a unit dedicated to the care of patients with both decompensated medical and psychiatric conditions.