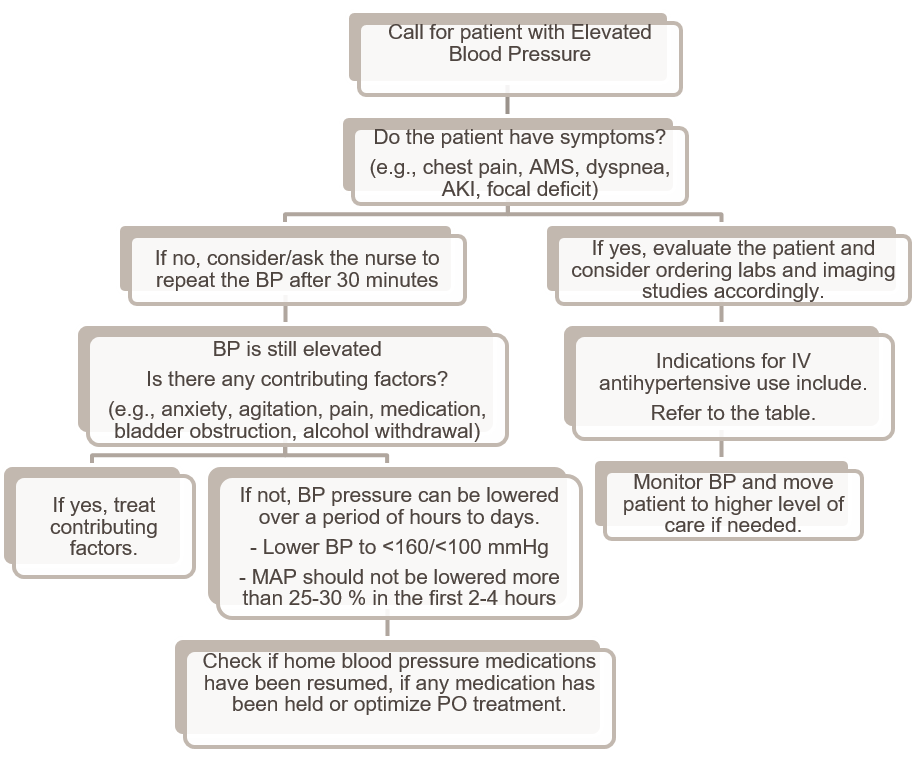
Background: Acute severe hypertension without evidence of end-organ damage (previously defined as hypertensive urgency) is a relatively common occurrence in the inpatient setting that can be frustrating and worrisome to both physicians and floor staff alike. Hypertensive urgencies have not been shown to be associated with increased short-term cardiovascular risk or mortality(1). Chronic hypertension is associated with a shift in the cerebral perfusion auto regulatory curve to the right, and these patients are susceptible to cerebral hypo perfusion when blood pressure is rapidly lowered(2). Management should be focused on gradual lowering of blood pressure over hours to days, after careful evaluation of secondary etiologies such as anxiety, pain, or withdrawal. Furthermore, the use of IV antihypertensive agents may lead to several adverse outcomes and they should not be used unless absolutely indicated(3). Nonetheless, hospitalized patients frequently have a PRN IV antihypertensive medication order.
Purpose: The goal of our quality improvement (QI) project is to reduce the ordering and use of unnecessary PRN IV antihypertensive medications by 20% across our community-based hospital over the next year.
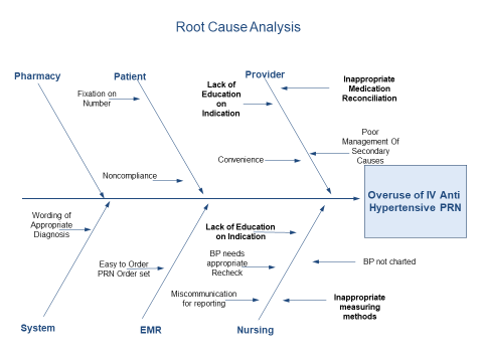
Description: At the start of the project, hospital wide data consisting of both Graduate Medical Education and private hospitalist medical teams, was collected to determine a baseline percentage and number of IV antihypertensive orders. Exclusion criteria consisted of appropriate indications for IV antihypertensive agents per 2020 International Society of Hypertension Global Hypertension Practice Guidelines. A total of 5339 inpatient encounters were recorded with a total of 992 administrations of IV hydralazine, labetalol or enalapril; the vast majority (88%) did not have an indication per previously stated guidelines and had BP of less than 180/110. Surveys administered to resident physicians showed that 36% of internal medicine residents believed that blood pressure should be managed with PRN IV agents. Nursing surveys showed that 100% of floor nurses were more comfortable with a PRN antihypertensive on the chart. Education regarding inpatient blood pressure management targeting resident physicians and floor staff were created and disseminated at academic sessions; quick reference guides were created and left at easily accessible locations throughout high-traffic resident and nursing work areas. Pharmacy and Information/Technology were contacted to assist in developing alterations to the current Electronic Medical Record, requiring selection of specific indications when attempting to order IV antihypertensive medications. Post intervention data is currently pending.
Conclusions: This resident-led QI project employed a multi-disciplinary approach to reduce the ordering of PRN IV antihypertensives for patients admitted to the general hospitalist service. Through the above-mentioned measures, we hope to see a significant reduction in the number of unnecessary orders for PRN IV antihypertensive agents.